Introduction
Thank you for having me again. I hope some of you were able to go to Part One, which was on pediatric bladder disorders. If you did not have a chance, I would highly recommend going back because it is so important to understand both the bladder and bowel systems when you are working with children.
Overview
- Bowel Disorders
- Behavioral Therapy
- Treatment Options
- Case Studies
- Resources and Practical Tips
I wanted to start by saying that the colon is probably more sensitive to psychological and emotional states than any other part of the body. I hope that this lecture helps you understand some of those things. Today, we are going to talk about bowel disorders, behavioral therapy, some treatment options, case studies, and then some resources and practical tips.
Bowel Control
One book I like is called "Understanding your Bowels" from the British Medical Association. I am just going to read this paragraph, and it is not in the slides. "In Western culture, the act of passing stools is an unfortunate necessity and an entirely private matter. As for the organs that produce stools, we prefer not to think about them. And if we do, we see them as mysterious, unpredictable, and rather disgraceful."
Why is this? There are grounds for some of these beliefs and attitudes. Stools are usually smelly, sometimes appallingly so. Diseases can be spread from people's stools to other people. The act of opening the bowels is an undignified affair, best done in private, and sometimes it is uncomfortable. The colon and rectum, which make the stools, are mysterious organs and perhaps the least understood organs in the body. Who has not been embarrassed by passing wind in others' company? I also love they say "wind" throughout that book. That is more of a British term, but anyway, I just wanted to start with that because who likes to talk about pee and poop? I know I do, but most people do not. This is something that I am passionate about.
Constipation and Urinary Symptoms
- 234 children – chronic constipation
- 29% daytime incontinence
- 34% nighttime incontinence
- 11% UTIs / 16% VUR
- Bowel Treatment program with disimpaction and maintenance
- Results:
- 52% constipation relieved
- 89% daytime dryness
- 63% nighttime dryness
- no UTIs
(Loening-Baucke, Peds 1997)
Many pediatric OTs and PTs are working with children, especially with issues of bowel and bladder control. I want to start with a study from 1997 that looked at two hundred and thirty-four children who had chronic constipation. Of those, 29% of those had daytime incontinence, 34% had nighttime incontinence, 11% had urinary tract infections, and 16% had vesicoureteral reflux which is when the urine backs up and goes the wrong way back to the kidneys. They did a bowel treatment program with disimpaction and maintenance. This resulted in the constipation being relieved. And when the constipation was relieved, daytime and nighttime dryness followed. The UTIs were taken care of as well.
- In a recent study of 73 children who received treatment for defecatory dysfunction (treatment not listed), 95% had resolution of symptoms.
- 68% of these children also had urinary incontinence. 50% of these children with UI had a reduction in the urinary incontinence just from treatment for the defecatory dysfunction.
(Borch, Hagstroem, Bower et al., 2013)
Constipation
- All children with bladder complaints have constipation until proven otherwise.
- Studies have shown that patients with voiding dysfunction have decreased sensation and increased tolerance to large volumes of stool in the colon.
- Parents are not aware of how infrequently their children are having bowel movements, and are unaware of the stool consistency.
- The contraction of the external urinary sphincter causes the contraction of the external anal sphincter.
- Defined as “unsatisfactory defecation with an "infrequent, difficult passage of hard, dry stool, or both” according to the American College of Gastroenterology
- < 3 bowel movements /week for at least 2 consecutive weeks
- Dyschezia-painful defecation
- Etiology can be multi-factorial, but in a “normal” child can be from painful defecation
- Other:
- decreased water
- decreased fiber
- decreased activity/playtime
- Mild dehydration is a risk for constipation
- Persistent stool in the rectum increases colonization of bacteria
- Increases the risk of UTIs in girls
- Becomes chronic
- Creates fecal retention
- Leads to stool withholding
- Encopresis
All children with bladder complaints have constipation until proven otherwise. I would say it happens 95% of the time. If you see a child with leakage or issues urinary-wise, typically, it is because they are constipated. Keep that in the back of your mind when you are working with these children.
Studies have shown that patients with voiding dysfunction have decreased sensation and increased tolerance to large volumes of stool in the colon. They get used to holding that stool, which stretches the nerves and the rectum. They do not get the sensation like they once did to go to the bathroom.
Parents are often not aware of how infrequently their children are having bowel movements, and they are not aware of stool consistency. The best way to know if someone is constipated is to look at the stool in the toilet. When I have kids and parents come to the office, I will ask the parent, "Is your child having a bowel movement regularly?" Sometimes, the child will pipe up and say, "No, mom, I only have one once a week." The parent(s) are usually surprised. The parents need to be curious about the child's bowel and bladder habits.
With constipation, contraction of the external urinary sphincter causes contraction of the external anal sphincter. If you are holding in urine, this is also going to have an impact on stool holding as well. Constipation is defined as unsatisfactory defecation with an infrequent difficult passage of hard, dry stool, or both according to the American College of Gastroenterology. It is less than three bowel movements in a week for at least two consecutive weeks. We will look at the consistency in a chart in a few minutes. Another part of constipation is painful defecation. Dyschezia is the medical term for that.
The etiology can be multifactorial, but in a normal child, it can be from painful defecation. The child may not be getting enough water. They also may not be getting enough fiber, activity, or playtime because the more active a child is the more regular their stools.
Mild dehydration is also a risk for constipation. Persistent stool in the rectum can increase the bacteria in the rectum. Thus, this can increase the risk of urinary tract infections in girls.
Constipation can also become chronic. Many of these kids will hold it and create fecal retention. When they do that stool-withholding, it is also called encopresis. They hold it in, it starts hurting, and they do not want to go. Often, they do not want to go to a public place. This becomes a negative pattern.
Transit Time
- Normal transit time in children is 48 hours
- Normal transit time in adults is 24-100 hours
Transit time is the total time from when we eat food to when it gets to the colon. The normal transit time in children is 48 hours. Normal transit time in adults is anywhere between 24 hours and 100 hours.
Encopresis
- Caused by constipation
- Reflexive withholding of stool by various psychological, physiological, or neurological disorders
- More common in boys than girls by a factor of 6:1
- If stool remains in the colon too long, the feces becomes hard as the water is removed from the colon.
- Painful for the child to expel
- The child avoids moving bowels for fear of anticipated pain.
- The rectal anal inhibitory response can result (anismus-dyssynergic defecation)
- Hardened stool builds and stretches the colon, and sensation associated with moving bowels is lost (megacolon).
- Softer stool leaks around hard stool creating diarrhea.
- A child typically has no sensation of episode
- Reduced rectal compliance
Encopresis is caused by constipation. It is a reflexive withholding of stool by various psychological, physiological, or neurological disorders. It is more common in boys than girls by a factor of six to one. Often, you will see children sitting with their heel against their perineum to try to hold that stool in. It can start as a control issue but then it can become an issue of pain.
The stool remains in the colon too long and the feces becomes hard as the water is removed from the colon. The longer it is in the colon, the more the body is pulling water from that stool. The child then avoids moving the bowels for fear of anticipated pain. There is also the rectal anal inhibitory response, which can result in problems as well.
Hardened stools are going to build and stretch the colon, and with that, the sensation associated with moving the bowels is lost. It is called megacolon or megarectum. In an x-ray, you can see that their rectum is completely stretched. The nerves in the rectum are compromised, and the child has no idea they have stool sitting in the rectum. The softer stool leaks around that hard stool, and so it looks like they have diarrhea. They will try to bulk up their child's stool when in fact they are constipated. They also can have reduced rectal compliance as they do not know that the rectum is full.
Childhood Fecal Incontinence
- Over the age 4 with leakage
- Encopresis
- Overflow incontinence
- shyness at school, sluggish colon, decongestants, painful fissures
- Pain-vicious cycle
- Paradoxical diarrhea-relaxed IAS and EAS, impaired sensation
- Megacolon and megarectum
- The Poo in You – YouTube video
We are also going to talk about fecal incontinence. You may be seeing adults that have fecal incontinence. I know in my practice I do as well. However, with kids, it is usually for a different reason. It is not that they are having weakness or tearing after delivering children. Instead, it is because they are impacted and the stools are leaking around it.
If a child is over the age of four and has any stool leakage, it is considered fecal incontinence. This is usually caused by encopresis, which is holding that stool in, and they can have overflow incontinence. They might be shy at school and afraid to ask to use the restroom, have a sluggish colon, or be on decongestants that can cause this. A painful fissure is like a cut in your lip. This can also happen in the anus, especially if a stool is really hard. It can create little cuts called fissures that hurt when the child has a bowel movement. As a result, they are more likely to hold stool in because they do not want to have that pain. This becomes a vicious cycle.
They can also have paradoxical diarrhea as a result of relaxed internal and external anal sphincters. I will go over those in a minute. They can also have impaired sensation or a megacolon/megarectum, like a stretched out balloon that does not have form anymore. It can take up to a year of a child taking MiraLAX or getting enemas to get that rectum to go back down to its original size. It is a very time-consuming and long process for these kids and parents. I highly recommend after we are done with this lecture that you go to YouTube and watch "The Poo in You." It is a great little video that shows a child with their parents in my office and I am explaining why they see little stains on the underwear.
Here is a picture of what is happening on the pelvic floor in Figure 1.
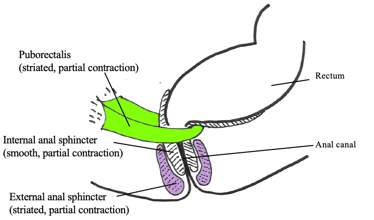
Figure 1. Puborectalis and sphincters at rest. (Picture used with permission from Louise Marks, OT)
Three muscles are important to look at in this picture. The puborectalis muscle is the one in green. This is a loopy muscle that helps us keep our stool and gas in. When sitting in an upright posture or at rest, it is partially contracted. It is also a striated muscle thus we do have control over it.
The internal anal sphincter (white with stripes) is a smooth muscle, like the bladder. It is not something that we necessarily can control, but it is partially contracted at rest. The external anal sphincter is in purple. This is also striated. You contract the external anal sphincter to hold in gas or stool if you cannot get to the restroom. The puborectalis, the internal sphincter, and the external sphincter are always partially contracted on their own even in rest.
The defecation reflex is shown in Figure 2.
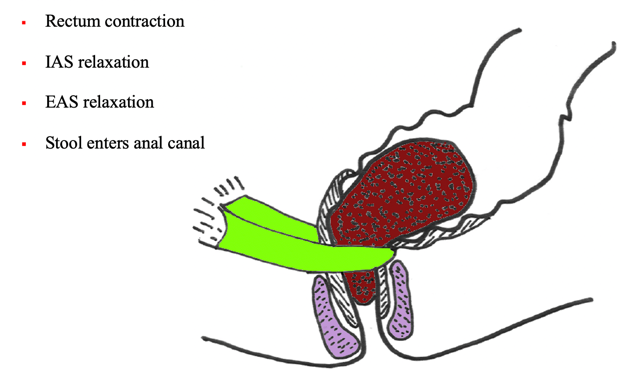
Figure 2. Defecation reflex. (Picture used with permission from Louise Marks, OT)
The rectum is contracting and pushing on that stool, which is brown. The internal anal sphincter (white muscle) relaxes. The external anal sphincter says, "Something's coming down the shoot so I'm going to relax as well." The stool then enters the anal canal. This is a reflex you feel when you feel like you need to go. If you need to inhibit this, you are going to actively contract the puborectalis muscle (see Figure 3).
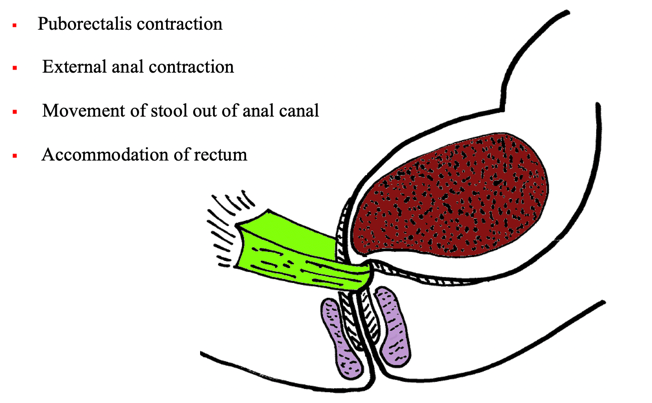
Figure 3. Inhibition of defecation. (Picture used with permission from Louise Marks, OT)
This muscle is attached to the pubic bone, wraps around the rectum, and comes back to the pubic bone. That is why it is called the puborectalis. You can also contract the purple muscle, which is the anus, to move the stool back up into the colon. The rectum will accommodate it and then relax so you do not have that feeling.
This can become a problem if a person does this too much. This can back up and goes a little bit further up into the colon. The longer it sits, the more the body is pulling water from it and it gets even harder. We call it "the call to stool." You need to go when you feel like it. With kids, it is a little more difficult because they are busy, they want to play, or they cannot recognize the signal anymore due to a megarectum.
When you do have a bowel movement, the rectum contracts and pushes that stool out. The internal anal sphincter, the puborectalis, and the anal sphincter all relax as shown in Figure 4.
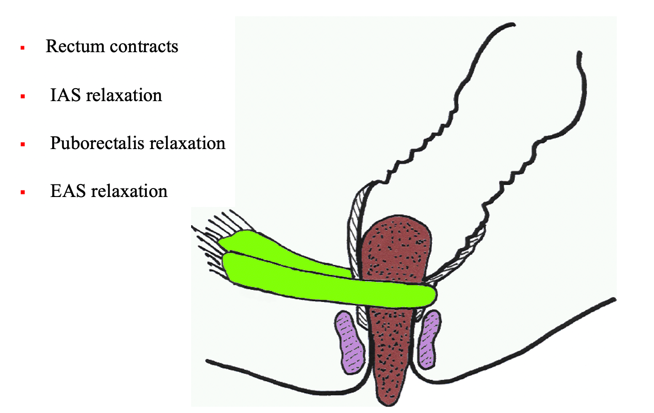
Figure 4. Defecation. (Picture used with permission from Louise Marks, OT)
Those muscles relax, but the rectum contracts to push that stool out. We do not have to think about this when we go to the bathroom. Sometimes, it is pretty easy, and we do not struggle too much. However, when you start having issues with bladder or bowel, it becomes more complicated and you realize how much work it is.
Bristol Stool Scale
This is called the Bristol Stool Scale in Figure 5.

Figure 5. Bristol Stool Scale.
They also have a scale for pediatrics that you can look up online. I like to show this to children and parents as I want them to look into the toilet. Most people find it is easy to recognize Type 1 as it is small pebbles that are easy to get out of. The problem is that this is the most constipated you can be. If the stool is separate, lumpy, and hard, this means that there is not enough water or fiber in the system.
You do not want Type 1, 2, or 3. Your goal is to be Type 4. It looks like a sausage or a snake, and it is smooth and soft. Sometimes, I describe it as a banana for kids. You want them to try to shoot for a Type 4. To achieve this, the child needs to drink a lot of water, eat food with fiber, exercise, and do many other things that we will talk about coming up.
If it is getting too loose, like a Type 7, especially with my adults, that is when they may have a lot of the stool leakage, especially with weak muscles.
I like to give calendars to the kids along with a colorful, bright, pediatric stool scale. I have them put it up next to a calendar that they pick out along with stickers. And then when they go, I want them to turn around and look in the toilet. I want them to mark the number on the calendar. We are hoping for 4's in the beginning. Sometimes I want the parent to come in as well. They can make it a game and each can guess what number to assign to it. This shows the parent how often the child is going and what the stool looks like. This is why it is very important to have both the child and the parent involved in this treatment.
Biofeedback and Behavior Modification as Treatment
Biofeedback and behavior modification is the best treatment for bowel and bladder issues. Behavioral therapy is outlined in Figure 6.
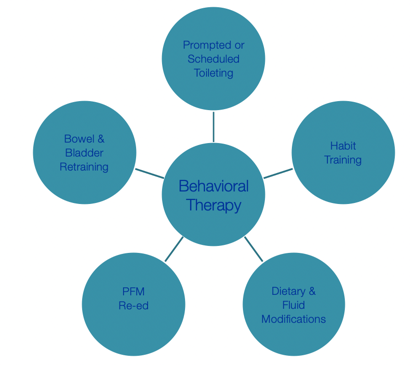
Figure 6. Overview of behavioral therapy components.
Sometimes, you have to put people on a schedule. There are tools to help with this, such as a wobble watch, that you can get on Amazon. This reminds the child to void (urine) every two to three hours. For habit training, you want them to go about the same time every day, if possible. You also want to look at both diet and fluid. Pelvic floor musculature (PFM) reeducation is also important.
Who is an Appropriate Candidate for Treatment?
- A child who is willing to participate in treatment.
- A child who can follow simple instructions.
- A family is willing to participate in treatment and make sure the child adheres (at least somewhat) to the toileting and medication schedule.
You need to have a child who is willing to participate in treatment. This is someone who wants to get better and cares about it as this will take some work. The child needs to be able to follow simple instructions. Additionally, the family has to be willing to participate in treatments and make sure the child is adhering to a toileting and medication schedule because this is going to be done mostly at home. They all have to buy into the process.
Behavioral Therapy
- Diet, Fluid and Lifestyle Modification
- Pelvic Floor Muscle Exercises
- Biofeedback
- Bowel and Bladder Retraining
- Home Program/Patient and Family Education
- Bowel and Bladder Diaries
- Toileting Posture
- Timer, Pager or Watch with Timing Intervals
During sessions, we are going to talk about diet, fluid, and lifestyle modifications, pelvic floor muscle exercises, biofeedback, bowel and bladder retraining, home programs and patient and family education, bowel, and bladder diaries, toileting posture, and equipment such as timers, pagers, and watches.
Elimination Diary
- How many times do you urinate every day?
- Do you use the bathroom at school?
- How wet are you during the day?
- Do you do the potty dance?
- How often do you have a bowel movement?
- When do you have a bowel movement?
- Describe your bowel movements.
- Do you soil your underwear?
There are many questions that you want to ask the child and parents. How many times does the child urinate every day? Are they using the bathroom at school? Many kids are embarrassed and do not use the restrooms at school at all. It could be inside the classroom, and the kids might hear them go. How wet are you during the day? Do they have some urine or stool leaks? Do you do the potty dance? This might be something that the parent can see especially if they are holding themselves with their hand. How often do they have a bowel movement? Again, most of the time parents do not know that answer, but the child can tell you. When do you have a bowel movement? Is it in the morning? Is it right when you get home from school or in the evenings? Describe the bowel movements. This is when I pull out the Bristol Stool Scale to show them. Is there soiling in the underwear? Many times the kids will hide their underwear. Other times, kids are not aware of the leaks, but other kids or parents can start smelling the stool. They might get teased at school or have a sibling tease them.
Dietary History
- What does a child eat in a typical day and when:
- Breakfast
- Mid-morning snack
- Lunch
- Mid-afternoon snack
- Dinner
- Before bed snack
What does the child eat in a typical day and when? Breakfast is extremely important, and we will talk more about that. Are they having a mid-morning snack, lunch, afternoon, or bedtime snack? What is their dietary history?
Fluid Intake History
- What does a child drink, and on a typical day?
- With each meal
- Between meals
- At school
- After school
- During sports
- After dinner
- Before bed
What does the child drink and when on a typical day? Are they drinking with each meal or between meals? Are they allowed to drink at school? What are they having after school? Are they having milk? Are they having Kool-Aid, Gatorade, and things like that? What are they drinking during sports, after dinner, and before bed?
Schedule
- Review the child’s daily schedule from the time the child gets up, to the time the child goes to sleep:
- When does the child void?
- When does the child move bowels?
- Use with a diet and fluid diary to get a complete picture of the day
I like to use a schedule that has times listed from 7:00 a.m., all the way up until bed. We talk about, "What time do you get up in the morning? What time do you go to sleep?" You need to get to know their schedule and also their bowel movements. You use this and the diary to get the complete picture of the day. You may not get a full picture the first time that you sit down with them, but over time, you will start to get a clearer picture if they use these tools. The weekends may look different than the school week. If they are from a split home, then the schedule is going to be a little bit varied as well.
Toilet Schedule
- Use a toilet schedule to prevent incontinence and help teach “mindful awareness” of body function
- Timed voiding
- Watch with multiple timers
- Coach/Teacher
- Parent
- Class schedule
- After school program
- Home schedule
The toilet schedule is important. You want to use a toilet schedule to prevent incontinence. If a child is holding for six or seven hours because they are nervous about going to the bathroom, they might have some leakage. You want them to start understanding when they need to go and to listen to the signals in their body. They might need to be on a timed voiding schedule. They might have to use a timer. The coach and the teacher might need to be involved. The parents may also need to be involved. When they go back to school, are they going to be able to have a break time? Are they going to afterschool programs? If so, this may be delaying them even more. We also need to look at the home schedule as well.
Treatment Goals
- Make goals attainable – don’t overwhelm
- Baby steps
- Celebrate accomplishments
You want to make their goals attainable. Do not give them too much information on that first visit. You might just want to have them start with getting a calendar. Their homework could be to go to the store and pick out a favorite calendar and some stickers. You want them to start thinking about how often they are going and have them try to follow a schedule for that first week. Perhaps they can also write down what they are eating and drinking. They can also pick out their favorite water bottle to encourage them to drink water.
You want to always celebrate their accomplishments. I like a little toy chest. If a child brings in their voiding diary, they get to pick from that toy chest and they get excited about it. Even if they do not fill it out perfectly, you want to celebrate that.
Commitment
- Establish a relationship with child and family
- Establish boundaries with child and family
- (no arguing about toileting)
- Establish goals with patient
- Ask the patient and family to commit
- Sign a contract if indicated
It does take a lot of commitment. Thus, you need to establish a good relationship with the child and the family and establish boundaries. You also want to make sure that there is no arguing about toileting. You want to establish goals with the patient to include what is important to them. They might want to get to the point where they can have a sleepover with their friends. Ask the patient and family to commit. "Let's sign a contract. You will be responsible for doing this, and then as a therapist, I will be responsible for doing my part."
Traffic Light Analogy
- Ask the child who is driving home today
- Ask the child what the driver is supposed to do at a red light
- What happens if the driver ignores the red light?
- See the importance of obeying a signal? (like the need to empty bladder)
- Ask the child what happens if she/he ignores the signal
I like to use a traffic light analogy. I will say, "What happens when you are sitting at a red light? You are supposed to stop obviously. What happens if your mom decides to ignore that red light, what can happen? There can be an accident. So, they need to obey that signal, just like it is important to obey the signal in your body. That's telling you, 'Hey, it's time to have a bowel movement' or 'Hey, it's time to pee.' Ask the child what happens if they ignore that signal? It might be that they do have a leak or they have an accident. This causes them to be embarrassed, or they might hide their soiled underwear from their parents or friends. They might not want to go to a friend's house because they are scared of this occurring.
Biofeedback
- Small electrical signal monitored with electromyography (EMG)
- Information about an unconscious process is presented visually on a computer screen
- Immediate knowledge of muscles becomes available to teach a patient how to alter the physiologic process
I love biofeedback. If you will be doing bladder and bowel training, I highly recommend that you learn biofeedback. I will talk about resources at the end but make sure the child understands their body. Biofeedback helps to teach them how to manage our bodies. Think of it like EKG for the heart and EMG is for the muscle. We are looking at muscle function, and it is information about an unconscious process that is presented visually. Kids love computers, and in a sense, they can play a game by making their muscles work to make the lines go up and down. They get immediate knowledge of their muscles in this way.
MEP probe.
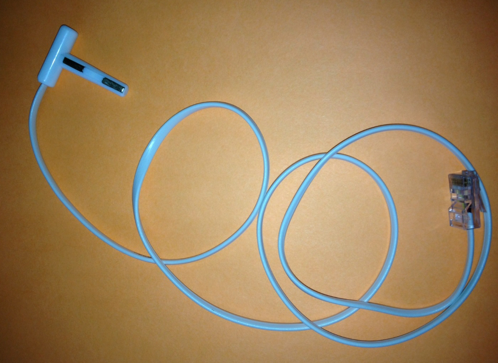
Figure 7. MEP probe.
This is an example of a type of probe. Pediatric urology office nurses typically use these. This is called an MEP probe, and it is very small. With adults, we can have them use internal vaginal or rectal sensors to read the pelvic floor muscles. With kids, I prefer to do external stickers right around the anus to be able to pick up the signal of the pelvic floor, but others, primarily nurses, will use really small devices, that go into the rectum. I prefer the external leads.
Figure 8, in the left-hand corner, shows a vaginal internal sensor, which of course is not used in pediatrics. This is used for adults. There is also a small vaginal or rectal internal sensor on the right. Below those is something with electrodes. This would be used outside of the body (bottom pic). You can use it for really any muscle in the body. It is not just for bladder and bowel control.

Figure 8. Different probes.
They do have disposable electrodes that look like the bottom option with the stickers already attached. That is just a onetime use that you would put on the child around the anus. Typically when I do bowel retraining, I have the child sit on the toilet. I have my laptop as well as a rolling stool with another laptop. I make sure that they have good support under their feet. I want them to void urine or stool while they are sitting on the toilet so it is very functional. The parent is also in the bathroom with us.
We teach them about breathing and how to have the bowel movement correctly. Figure 9 shows an adult, but I wanted to show how you can set up either the rectus abdominis, which is right under the belly button, or the obliques.
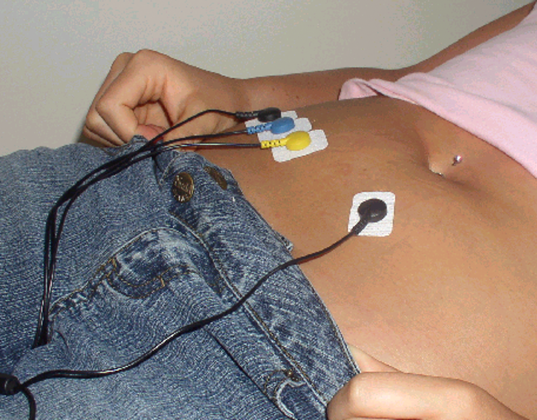
Figure 9. Electrodes on the abdominals and obliques.
The abdominals are an important muscle group for them to learn how to use when having a bowel movement. These are the muscles that are contracting and helping push the stool out while the pelvic floor muscles need to relax to release the stool.
Figure 10 shows an example of a biofeedback graph and what it would look like when someone has constipation.
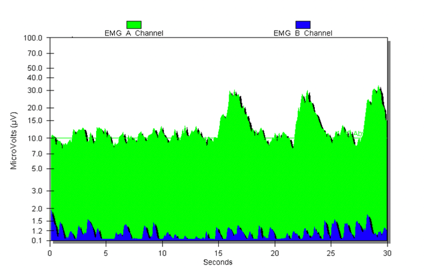
Figure 10. Biofeedback graph showing constipation.
The green line is the pelvic floor. The stickers placed around the anus are picking up the tension in that muscle. This is why there is a lot of activity on the screen. The blue lines represent the abdominal muscles.
In Figure 11, I am teaching the child that rather than having a constant contraction of the muscle to instead contract and release the pelvic floor muscles. This is like a Kegel exercise in adults.
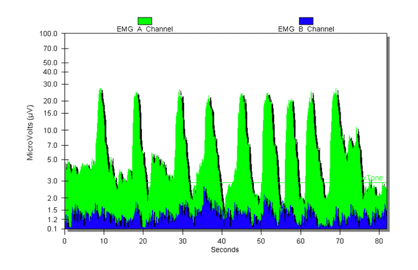
Figure 11. Biofeedback showing contraction and release of the pelvic floor muscles.
They are contracting the pelvic floor, which is contracting the anus, vagina, and urethra. During contraction, the green line would raise, and during relaxation, it would go down. In contrast, many children are using constant tension in the muscle as in the first graph. If you do not have a range of motion in that muscle and you are just holding all the time, then the stool is not going to come out because you cannot release it.
Biofeedback teaches them how to understand this. We call them the "potty muscles." "If you squeeze like you are holding in gas (fart, toot, etc.), that line will go up. If you release, that line will go down."
Many biofeedback machines have visuals like a dolphin that is jumping or a puppet going up and down. It does not have to be a very fancy machine, but you do want them to have the ability to see it on a computer screen. This child got the hang of the potty muscles and how to contract and release them.
Behavioral Therapy and Biofeedback Treatment
- Education regarding voiding and bowel function
- Elimination education:
- Increase fluids
- Timed voiding, voiding strategies
- Bowel program
- Hygiene
- Biofeedback: helps children identify and relax appropriate muscles for elimination
- Monitoring 2 channels is critical to success
With behavioral therapy and biofeedback treatment, we are trying to educate them regarding bowel function. Elimination education does include talking about increasing fluids. Of course, you want more water, intake, timed voiding, and making sure they have strategies, like a bowel program, which we will talk about. We also want to talk about good hygiene. We do not want them to leave stool sitting in their underpants as this can cause a UTI as the E.coli bacteria can go up into the urethra.
Biofeedback, again, helps a child to identify and relax the appropriate muscles for elimination. For this, you want to monitor two channels. Many people use a handheld device, but it is just a one channel EMG and it takes coordination. The whole point of teaching a child how to have a bowel movement is they have to learn how to coordinate the abdominals and the pelvic floor. For this reason, I suggest two channels and the use of the software. It does cost a little bit more, but a child just holding a box seeing a line going up and down is not going to give as much information as a two-channel system with software.
- Down-play incidents
- Provide positive incentives
- A child needs to learn responsibility for self-care
- Should be a primary treatment in children with voiding dysfunction
- Parents tend to downplay constipation or are unaware of the child’s bowel patterns
You want to downplay the incidents. If they are having a lot of incidents, you want to provide a lot of positive incentives for the child. Like we discussed in the bladder section, if someone has a bedwetting issue, you may want to use a chart and stickers. For example, if they do not have any incidents for two days, they get an incentive. This is the same as a bowel program. You are providing incentives with the parent as well. The child needs to learn responsibility for self-care, and biofeedback should be a primary treatment in children with voiding dysfunction.
Treatment Impact
- Strengthen appropriate muscles
- Inhibit uninhibited contractions
- Learn how to relax the pelvic floor
- Neuroplasticity
- Reset coordinated function (CNS/local)
- Educate/treat
With biofeedback, we want to strengthen the appropriate muscles and help them understand the process. We want to inhibit uninhibited contractions. Sometimes people will have bladder urges or sensations, and it is an uninhibited bladder sensation causing the person to go frequently to the bathroom. We want to inhibit these sensations by teaching them how to relax the pelvic floor and release that tension. When you are doing biofeedback, you are creating neuroplasticity and teaching the brain and the muscles what they need to do for proper elimination. You are resetting that coordinated function.
Treatment Strategies
- Monitor muscles and teach during active voiding
- Teach isolation and relaxation without voiding
- Teach muscle coordination for proper elimination
- Teach proper toilet posture
- Make it fun for the child!
- Teach to the level of the child, not the parent
You want to monitor the muscles and teach during active voiding if you are able. I have worked in places where I did not have access to a restroom. Now I do which is great because it teaches the child in realtime how to eliminate properly. You are teaching isolation and relaxation without voiding. If you are sitting in the office, you want them to understand to squeeze the "potty muscle" and then let it go. You can do the biofeedback without sitting on the toilet to give them the same information.
They need to be in a proper position with good posture. You also want to make treatment fun for the child. If I am teaching breathing, I might have them blow up a balloon, blow on a pinwheel type fan, or use bubbles. Remember that you are teaching to the level of the child, not to the parents so you want it to be fun and engaging.
Indications for Biofeedback
- Abnormal flow pattern
- EMG activity during voiding
- Significant PVR
- Inability to initiate flow in the absence of urgency
- Poor bladder emptying (UTI)
- Retraining after surgery/trauma
If the child has an abnormal flow pattern, this might be a reason that a physician is referring them to you. We talked a little bit about that with the bladder section. If they are having EMG activity during voiding, this means that they have increased activity in the muscles of the pelvis when they should be relaxed during voiding. We talked about how a balloon is a bladder and the knot represents the muscles. Their muscles are knotting when they are supposed to be relaxing. They might also have significant post-void residuals. There is too much urine still in there after voiding. Or, they may not be able to initiate the flow. If they are not getting good bladder emptying, they can incur urinary tract infections. And sometimes, they need retraining after surgery or trauma.
Pediatric Biofeedback
- Case study reports improved continence following intervention with biofeedback for pelvic floor muscle dysfunction in a five-year-old child.
- Surface EMG biofeedback perineal electrodes were used during treatment sessions to provide visualization of muscle.
“Biofeedback-Assisted Muscle Training for Pelvic Floor Dysfunction to Address Pediatric Incontinence: A Case Report”. Gibbs, K., Kenyon, L., Journal of Women’s Health Physical Therapy, January 2018: 17-22.
There was a case study done that reported improved continence following intervention with biofeedback for pelvic floor muscle dysfunction of a five-year-old child. While this child seems young, many five-year-olds can follow simple instructions. They can look at a screen and know, "If I squeeze this green line goes up. If I relax, it goes down." Surface EMG biofeedback perineal electrodes, which means they are on the outside, are used during treatment sessions to provide visualization of the muscles, which is very important for these younger ages.
Lifestyle Interventions
- Fluid and Diet Modification
- Prevention
- Weight Loss
- Exercise
- Relaxation/Yoga
- Nocturia Management
- Facilitate Voiding and Bladder Emptying
- Treat the Constipation
Again, fluid and diet modifications may need to be made. You may need to look at prevention and weight loss as well. Sometimes with weight loss, this takes the pressure off of the pelvic floor for better emptying. Exercise is really important. It helps with peristalsis and getting the colon to move. A lot of kids need some relaxation if they have ADHD or they are very hyper. They tend to not be able to focus on what they need to do or do not get the signals from their body. They need to learn to get more in tune with their body. Nocturia management means decreasing the number of trips to the bathroom a night. We want to look at their nighttime behaviors and facilitate voiding and bladder emptying on good time schedules. The most important thing is to treat constipation. Do not forget that. If anyone comes in with a urine issue, I can guarantee you they have a bowel issue, or they are constipated.
Lifestyle Modifications
- Bowel habit regulation
- Regular and predictable
- Adequate fiber
- Avoid straining
- Adequate fluid and exercise
- Regular time
- Heed the call – listen to your body!
- Avoid constipation
You want to regulate their bowel habits by getting them on a good regular schedule. It needs to be regular and predictable. For some kids, they may need to get up 20 minutes earlier and eat immediately so that their body has time to have a bowel movement. If they are rushed, they may not have the proper time to sit and have a bowel movement. They need adequate fiber. It is recommended for really young children, ages two and three, to be at about 14 grams. A child between ages four and eight need around 20 grams of fiber. From age nine to teenage years, they need the same as adults, so at about 25 to 35 grams of fiber.
You also do not want kids to strain to have a bowel movement. I have seen kids in the past that strain so much that they have had a prolapse. The rectal wall will fall because of this. They want to have adequate fluid and exercise going on to reduce this straining. Try to get them to listen to their body. I have teenage boys. If they are heading into the restroom, I make them leave their phone. If they have the phone in there with them, they might take 30 minutes, but if I take the phone away, they are in and out in about three to five minutes. Many kids get distracted when they are playing a game, and they are then not in tune with their bodies.
Toilet Posture
We have talked a lot about toilet posture. Let's take a look at this in Figure 12.

Figure 12. Correct toilet posture.
We discussed the different muscles that are in the pelvic floor. The puborectalis muscle is the "loopy" muscle. If you are sitting upright with your knees in a 90-degree angle, that muscle is kinked. And, often kids dangle their legs because their feet are not supported. When they are not supported, they may feel like they are falling in the toilet and often have a hard time balancing. Because of this, they might be contracting their pelvic floor muscles and adducting their knees. All of this muscle contraction is not going to allow proper elimination. On Day 1, their homework is to get a Squatty Potty. You can get them on Amazon, Target, or Bed Bath & Beyond. It is not a regular stool because the knees cannot be touching. You want the knees to be separate. Make sure the child also pulls their shorts or their pants down to their ankles. If their pants are around their knees, then they tend to be internally rotated and their adductors are going to be activated. You want them to be supported and feel that they can relax and be comfortable.
Fluid and Diet Modification
- Eliminate or reduce bowel or bladder irritants
- Modify timing and amount of fluid intake
- Modify bowel habits
You want to eliminate bowel and bladder irritants if that is causing a problem, and we will go over those in a minute. Again, we want to time and control the amount of fluid intake. Lastly, we want to modify the bowel habits.
Common Bladder and Bowel Irritants
- Caffeine
- Chocolate
- Citrus Products
- Artificial Sweeteners and colors
- Spicy food
- Tomato products
- Vitamins B, C
- Soda
- Milk or dairy products
- Sugar
Caffeine, like in soda, is your number one problem and the biggest bladder irritant. It is a stimulant. I am hoping young kids are not having any caffeine, but they might be. Chocolate also has caffeine. Sugary items also irritate the bowel and bladder. Anything citrusy can also cause problems as well as things with artificial sweeteners and coloring. These would be things like Kool-Aid, spicy foods, tomato products, and vitamins. I still want children to take vitamins, but they do should not take them before bed because that will get them up in the middle of the night. Milk and other dairy products are also problematic.
Abdominal Massage
I want to talk a little bit about abdominal massage. It is fantastic especially if a child has constipation. We have to get the peristalsis going because they have a slow gut. The first example is shown in Figure 13.
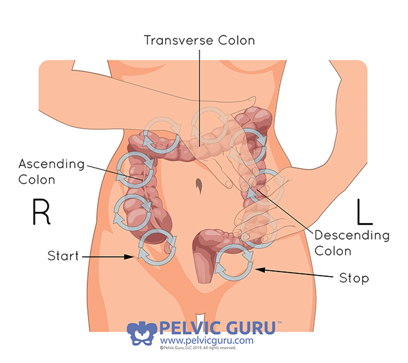
Figure 13. Abdominal massage.
On the left-hand side of the body is the ascending colon. As food travels from the stomach, it goes through the small intestine to the large intestine. It goes up the ascending colon, and that is where it is fermented. It then goes across the body in the transferase colon. This is where water and the salt are removed. Food is stored in the descending colon, which is along the left side of the body going down. Lastly, the sigmoid colon makes a little loop down towards the base and the rectum. The sigmoid colon is named after the squiggly Greek letter Sigma. The rectum is a Latin word that means straight.
You do want to do certain circular movements and you want them to go clockwise because you want the stool to go up, over, and down. So you're trying to create that peristalsis to get things moving. So if a child is backed up and uncomfortable, or they have gas, this massage is great. So you can teach the parent how to do it. You can also have the child do it. An example of an abdominal massage is called, "I love you", as displayed in Figure 14.
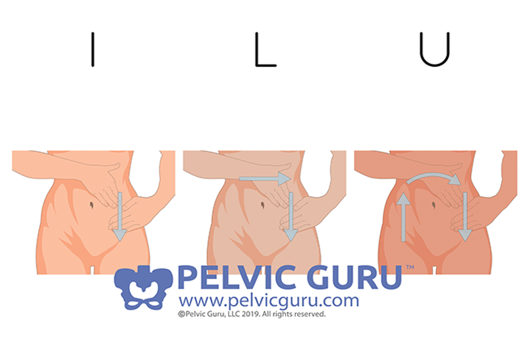
Figure 14. "I love you" massage.
You have them start at the descending side to create the "I." They are going to massage straight down, and they can do those circles. Then, they are going to go to the transverse colon, go across the body from their right to the left rib, and then down which creates an upside-down "L." To create the "U," they are going up the right side of the body, over to the left rib, and down the descending. They can do this anywhere from 10 to 20 minutes. Sometimes the kids think it is fun. Let's say they have some gas bubbles in there, it might feel as if they are popping little gas bubbles. Sometimes, they can even feel the stool that is sitting in there. Both of these methods can help them with discomfort.
Hydrate
- One ounce of fluid per 2 lbs. of body weight
- The child weighs 60 lbs.: they should drink 30 ounces
Hydration is important. For a child, they need one ounce of fluid per two pounds of body weight. If you have a child that weighs 60 pounds, they should be drinking 30 ounces. This is the same formula for adults. If you have an adult that weighs 120 pounds, they need to drink 60 ounces of water. A lot of people think, "Coffee and tea are included." However, tea and coffee can dehydrate the body and can cause constipation. You also do not want them to add Crystal Light or Kool-Aid to the water. We want plain water. As an incentive, you can use a calendar or a new water bottle. For example, if they are a 60-pound child, their goal is to finish a 30 oz. bottle throughout the day. Remember, you do not want them slamming it down in five minutes. Instead, you want them to sip on it slowly so they are getting the benefit and not just peeing it out.
Benefits of Drinking Water
- Urinary diuresis greatly reduces the count of infection in the urine
- The optimal functioning of our body requires a good hydration level
- Water fills the bladder efficiently, giving the child “reason to void”
Urinary diuresis greatly reduces the count of infection in the urine. The optimal functioning of our body requires a good hydration level, and water fills the bladder efficiently. Then, the child can feel that they need to void.
Success
- Urinate often
- Drink lots of water
- Move your bowels daily
- Be aware of when your body tells you it is time to empty
- Don’t argue with your parents if they tell you it is time to use the toilet.
For success, you want them to urinate often. This is between two and three hours. You want them to drink lots of water. You want them to move their bowels daily and be aware of when their body tells them it is time to empty. You do not want them to argue with their parents when they say it is time to use the toilet.
Diet and Lifestyle Modification
- Bowel Habit Regulation
- Goal: Regular and predictable
- Adequate Fiber (20-25 grams a day)
- Avoid straining
- Fluids and Exercise
- Regular time
- Heed the Urge
- Avoid constipation
- Take fiber supplements/laxatives as prescribed by a physician
For bowel habit regulation, the goal is regular and predictable. You want them to avoid straining, have good fluid, exercise, and go at a regular time. You want them to heed the urge to void constipation. Some may need to take fiber supplements. I do not recommend laxatives, but if an MD suggests that they need to discuss that. Many physicians prescribe MiraLAX, while others would rather do suppositories. All this needs to be discussed with the primary physician.
Case Studies
So let's look at a couple of case studies.
Dylan
- Nine-year-old girl. Lives with her mother. Parents divorced. Experiences urinary frequency and incontinence.
- Moves bowels 2-3 times a week. Type I to IV Bristol Stool Scale.
- Mother is getting counseling for herself for anger management. Dylan’s urinary incontinence makes her mother angry, and this interferes with the mother/daughter relationship.
- Dylan wets his pants several times a day.
- Teachers won’t let her use the toilet at every request, as they feel this is behavioral and disruptive to the class. They think Dylan uses toileting as an excuse not to do work.
The first one is Dylan. She is a nine-year-old girl. She lives with her mother as her parents are divorced. She is having a lot of urinary frequency and incontinence, which is the leakage. She moves her bowels two to three times a week, and they are the type I to IV, but usually more like I and II, which were those pebbles. Mother is getting counseling for herself for anger management as the incontinence of her daughter is making her angry. It is also interfering with their relationship as they are fighting a lot about it. Dylan is wetting her pants several times a day, and the teachers are not letting her use the toilet at every request because they think she is being disruptive and using toileting as an excuse. While there might be some kids that do that, for the most part, they need to go.
- Detailed history with bowel and bladder diary requested. Discussed anatomy, good fiber, use of fluids. “The poop drives the pee.”
- Biofeedback to teach Dylan what muscles do, and why and how they are the gatekeeper to elimination.
- Proper toileting posture and adequate time on the toilet
- Electrical stimulation for OAB symptoms
A detailed history with a bowel and bladder diary was requested. We talked about pelvic anatomy, good fiber, and the use of fluids. "The poop drives the pee. If you can get the poop moving, then usually that takes care of the pee issues." We watched some of those videos together. She loved biofeedback and learned what those muscles do and how are they the gatekeeper to elimination. Of course, I recommended a Squatty Potty for good positioning and support. We also talked about how 20 minutes after a meal is the best time for a child to see if they can go.
Many people ask if you can do electrical stimulation. Some children cannot feel the muscles or they are not sure what to do, you can do a little bit of external E-stim. This would be set low so that they would just feel some tingling in the appropriate areas. You do not have to do that with many children, but it is an option.
- No symptoms
- No problems with toileting at school
- Mother and daughter in counseling
- Both happy and getting along
- Thrilled with the progress
- 10 visits
After going through all the therapy (10 visits), there were no symptoms. She also was not having problems with toileting at school. She and her mom both began counseling. Of course, we can work on many issues, but counseling is recommended in these instances. They both were really happy with the process.
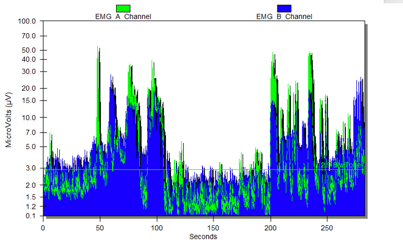
Figure 15. Dylan's first graph.
This was some of the EMG. Remember the green is the pelvic floor, and the blue is the abdominals. She had a lot of fighting between the two muscles, and they were not very coordinated. She could not figure out how to use the pelvic floor. I usually say, "Hold in gas. Let go of the gas." This is what the child understands. If you look at the post-treatment in Figure 16, she was able to relax her belly when I was asked her to contract her pelvic floor.
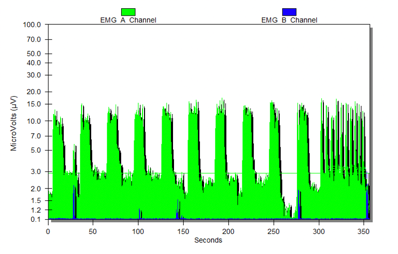
Figure 16. Dylan's second graph.
You can also see that she had a good range of motion. I am asking her to hold and then release. She made me this cute picture in Figure 17 as a thank you.
Figure 17. Dylan's note.
"You helped me with butt promble (problem)." I get very cute little letters and pictures all the time.
Nick
- A fifteen-year-old boy lives with his father and his new wife. Nick doesn’t get along with the new wife.
- H/O ADHD. He was on Adderall, but Nick took himself off the drug stating he wanted to learn how to control things without the use of the drug.
- Doing well in school, although some motivational issues according to his father.
Nick is a 15-year-old boy who was living with his father and new wife. He did not get along with his stepmom and has also had a history of ADHD and was on Adderall. He reported not liking how he felt while on it. He did not want to use it. He was doing well in school, but he had some "motivational" issues, according to the father.
- Referred by a pediatric gastroenterologist because of encopresis.
- Now taking Miralax but still experiencing incontinence.
- Unaware of muscles or when he gets his call to stool. Unaware of when he has his accidents.
- Faithful with his bowel diary. Interested in anatomy and learning about his body.
He was referred by a pediatric gastroenterologist because of the encopresis in the holding of stool. He was also on MiraLAX, but he was still having some incontinence. He was unaware of his muscles or when he had a "call to stool." He was also unaware of when he was having his accidents. Usually, if they are constipated, they have a few accidents. They do not feel the way they used to feel. He was faithful about his bowel diary and really was very interested in his anatomy and just learning about his body.
- Nine visits later he knew he would need to move his bowels right after school, and again around 8 PM. No longer using Miralax, but taking gummy fiber and eating healthy meals.
- Father and stepmother had trouble with his learning style: always came up with chore ideas when it was time for him to use the toilet. If he was distracted with their “tasks” he had an accident. Sometimes it is more about teaching the parents!
Nine visits later, he knew he needed to move his bowels right after school. And again, he would after 8:00 p.m. He was able to figure out what his system was doing. He started taking gummy fibers and eating healthy meals. His father and stepmother had trouble with his learning style. They were always coming up with chore ideas when it was time for him to use the toilet. When a kid is distracted, sometimes they will have an accident. In this case, I had to teach the parents. I also had to encourage them not to punish if he was having issues. Figure 18 shows his first graph.
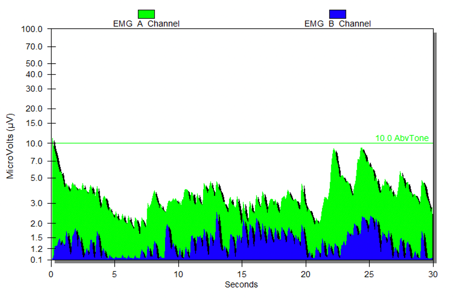
Figure 18. Nick's first graph.
This is just an example of pre-treatment where he was trying to figure out his muscles. Again, there are many different types of screens you can use. There is even a guy jumping over a high jump. However, I like to use the line. You can see his post-treatment and where the line is in Figure 19.
