Learning Outcomes
After this course, participants will be able to:
- Describe at least three steps in the process used to develop the Berlin concussion consensus statement.
- Identify at least two best practices according to the Berlin concussion consensus statement.
- Identify at least two sources of evidence supporting the Berlin recommendations.
Introduction and Overview
Today's presentation is going to be an overview of the concussion management recommendations that came from the Berlin Meeting, which took place in October of 2016. The way that I have organized today's presentation is to first talk a little bit about the consensus statement development process. I think it's important as clinicians that we understand what goes into these types of documents, the rigor with which the evidence is evaluated to develop certain recommendations, especially for a topic like concussion that garners a lot of attention, not only in the medical literature but also in the lay media. We're going to provide an overview of the consensus statement and review the recommendations, which were developed in this series of 11 Rs. We'll go through each one of those, hit on some of the evidence supporting those and what are the future directions and the elements that might be most important to your clinical practice? Because of today's audience, we're going to spend a little more time focusing on some of the recommendations related to treatment and rehabilitation and returning individuals to sport participation.
Lastly, I'm going to talk a little bit about concussion statement use in clinical practice. This is the most recent statement but it's certainly not the only statement. I think as healthcare providers, it's always good to have a different understanding of what types of consensus and position statements are available for different stakeholder groups, how are they similar and perhaps how are they different. When we talk about concussion and the need to manage it within the context of an interdisciplinary healthcare team, I think it's important for physical therapists to understand what the neurologist's statement says, and for athletic trainers to understand what the neuropsychologist's statement says, because if there are differences in how it's being managed, it doesn't necessarily mean it's right or wrong. It could just be the views and the recommendations of some of those different healthcare providers in how they're interpreting the evidence for their own clinician stakeholder group.
Clinical Practice Guidelines
Clinical practice guidelines are systematically developed statements to assist practitioner and patient decisions about appropriate healthcare for specific clinical circumstances (Institute of Medicine, 1990). They're often developed to improve the quality of patient care and are typically developed based on experience and judgment. However, in recent years, there has been a shift in focus towards evidence-based clinical guidelines.
Clinical practice guidelines are developed and implemented for a number of different reasons which benefit clinicians, patients, and the healthcare system. These guidelines are instituted to describe appropriate care based on the best available scientific evidence and broad consensus. They also help to get everyone on the same page in order to reduce variation in practice, in some cases inappropriate variation. Clinical practice guidelines provide a rational basis for referral, as well as providing a focus for continuing education needs for clinicians. They promote efficient use of resources, act as a focus for quality control (including audit), and they highlight shortcomings of existing literature and suggest appropriate future research. With this consensus statement, in particular, there are 12 systematic reviews of the literature that support the recommendations made. For anyone who mentors students, or if anyone is looking for potential research projects, those systematic reviews can provide an abundance of information on what researchers need to be collecting, evaluating, analyzing, and publishing.
Benefits of Guideline Use
When we look at the benefits of clinical practice guideline use with respect to our patients, it should result in a better quality of care and improved health outcomes, as well as the improved consistency of care across different clinicians in different geographic regions. There should be an educational component to help inform patients about decision making and empower them in decision-making for their own healthcare. Clinical practice guidelines can be used to influence public policy and promote distributive justice across different patient groups.
From a healthcare provider standpoint, the guidelines can help us make better quality clinical decisions, and reassure us that our practice is appropriate. It can provide explicit recommendations to guide care and to reduce outdated, ineffective or wasteful practices. The guidelines help providers to support quality improvement initiatives, as well as to inform the research agenda by identifying gaps in evidence.
At the healthcare system level, the use of clinical practice guidelines should help to improve efficiency and optimize value. Additionally, demonstrating adherence to guidelines may improve a healthcare system's public image.
Types of Clinical Practice Guidelines
The types of clinical practice guidelines available can be broken down into four categories: expert consensus, evidence-based, outcomes-based and preference-based. Today, most of the guidelines available for concussion fall somewhere between the expert consensus and the evidence-based guidelines.
- Expert consensus guidelines are based on the opinions and recommendations of experts or leaders in a certain profession. It may be somewhat based on the evidence, but they're often based on the opinions. These guidelines have a lower level of applicability and may reflect biases in those particular experts and their professions.
- With evidence-based guidelines, the rules for identifying and assessing evidence are determined prior to searching for evidence. There are a specified means of translating the results of studies into a recommendation.
- With outcomes-based guidelines, we collect outcomes to assess the effectiveness of the evidence-based recommendations and determine whether or not they improve the quality of care for our patients. This can include meta-analyses, decision analyses or cost-effective analyses as part of the guideline development process.
- Preference-based guidelines take into account the values of patients. If we think about the evidence-based practice paradigm, that third leg of the stool is patient values and includes the patient values in the decision-making process.
Concussion Statements
Why are there so many statements and why do we have all of these different and, in some ways, contradicting recommendations? A lot of concussions occur annually (between 1.1 and 1.9 million per year). Over one-third of those concussion cases are seen in the outpatient care setting as their primary point of entry. Other people choose to go to the emergency department, usually younger individuals and children. Some concussion cases are managed primarily through the school setting, in secondary schools where there is an athletic trainer. Because of all of the attention focused on concussion, we've seen a series of different consensus guidelines being developed over the years. Some of them replace each other; they're updated as newer evidence is provided.
The first international guidelines were published in 2001 following a meeting in Vienna (Figure 1). The National Athletic Trainer's Association (NATA) published their first concussion position statement in 2004. Subsequent international statements were published in 2005 (Prague), 2009 (Zurich) and 2013 (Zurich). The National Academy of Neuropsychologists (NAN) published their first paper in 2007. The American Medical Society for Sports Medicine (AMSSM), the primary care sports medicine trained providers, had their guidelines for physicians published in 2012. The American Academy of Neurology (AAN) had theirs published in 2013. It is important to note that the AAN did follow an evidence-based guideline process; these are the first and only that are truly evidence-based guidelines. With the exception of the AAN, most are consensus (expert) or position statements. NATA did recently update their 2004 statement, and their revised statement was published in 2014.
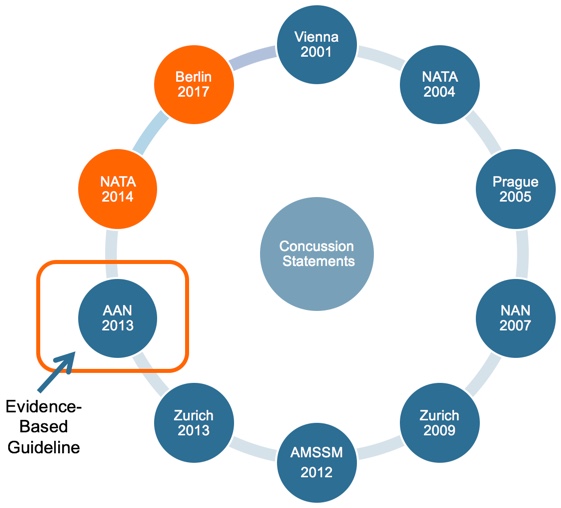
Figure 1. Concussion statements.
Today, although we will be focusing on the Berlin document and guidelines for 2017, it is also important to understand the history and how some of these documents may be similar or different.
