Kathleen: Thanks everyone for joining us. I hope that this is a well worth your time, and that you get a lot out of today's session. This is part one of a two part series. Today's presentation is focused on the reasons why we use water as a modality in our clinics.
Overview
Thanks everyone for joining us, and I hope that this is a well worth your time, and that you get a lot out of today's session, and this is part one of a two part series. Today's presentation is focused on the reasons why we use water as a modality in our clinics. The use of water as a healing agent has been around for thousands of years. This is nothing new, but as therapists we should know some of the basic concepts of water to effectively and safely treat in the water. We will discuss the principles of water, and how those impact our patients and treatments. Our system review will include a circulatory system, pulmonary system, the musculoskeletal system, and the renal system. We will review these systems of the body, and we will learn how they are impacted by the principles of water. We will review the important physiological impacts that we need to know in order to treat our patients safely in the water. You will be presented with a list of precautions and contraindications that you should understand before you begin an aquatic therapy treatment plan. Then, we will discuss the therapeutic benefits that will aid your patient's recovery process. I will give you an example of a case study, and how I have used the pool to facilitate function and restoration of his impairments. It is important that we are able to take what we do in the pool and translate that to how it is impacting their ability to complete ADL and functional mobility, or as I say, "We need to make them better on land." Insurances will not want to pay for something that does not impact our patient's normal routine of life. In order to justify these plans of care, we need to be able to show measurable, functional progress. I hope that if you are new to aquatic therapy, that after we are done today, you are able to see clearly how the water can truly impact the overall function and abilities of your patients. If this is an area that you are currently practicing in, I hope that today you will take back to your clinics a few key items to add to your clinical toolbox.
Principles of Water
Hang in there with me, as I know some of the science behind the water is not as much fun as treating in the water, but I feel strongly that it is important for you to know these principles, and especially how they impact your patient's treatments. I think your patients would appreciate you teaching these principles to them so that they can understand why we do what we do in the water.
Buoyancy
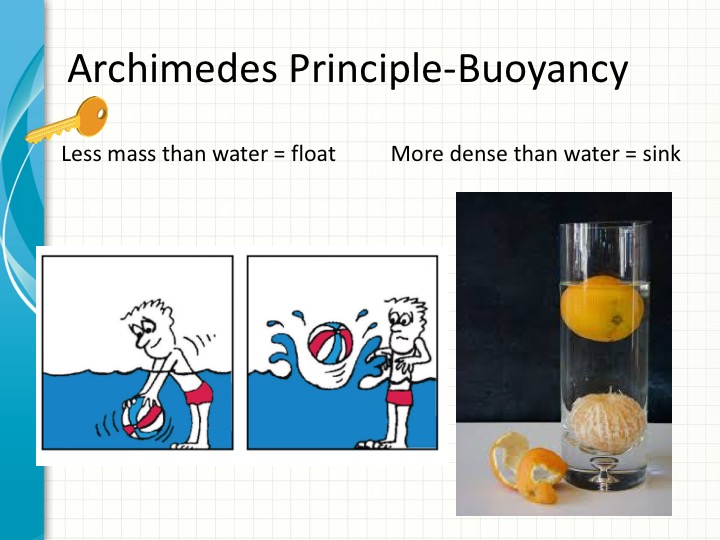
Figure 1. Overview of buoyancy.
According to the Physics Hypertextbook, buoyancy, or the buoyant force, is the force that is exerted on an object that is fully or partly immersed in a fluid. Buoyancy is caused by different pressures acting on opposite sides of an object immersed in a static fluid. The pressure on the bottom of the object is greater than on the top. The force on the bottom pushes up, and the force on the top pushes down. The direction of the net force due to the fluid is upward. Translating that to our treatment in the pool means that buoyancy will assist our patient's movement upward towards the surface of the water, and the buoyancy will provide resistance in a downward direction from the surface of the water. Buoyancy is the force that causes an object to float or sink. When you are immersed in water, you feel that you are lighter and more buoyant. The general concept that governs floating and sinking is called Archimedes Principle. An object immersed in liquid experiences an upward force called upthrust or buoyancy according to this principle. Also according to Archimedes, when a solid is placed in a fluid, it is subject to an upward force equal in magnitude to the weight of a fluid it has displaced. Floating or sinking of an object does not depend on its weight, but on its density. Things denser than water sink, whereas things having less mass than water float over it. While our patients are submerged in water, the buoyancy reduces the force of the stress placed on their joints, and it typically makes it less painful for them to perform active range of motion or exercise. The buoyancy allows our bodies to feel weightlessness, and this unweighting of the joints is one of the greatest benefits of therapy in a pool.
Hydrostatic Pressure
According to dictionary.com, hydrostatic pressure is the pressure exerted by a fluid at equilibrium at any given point. Due to the force of gravity, hydrostatic pressure increases in proportion to the depth measured from the surface because of the increasing weight of the fluid exerting downward force from above. I think Figure 2 does a nice job of explaining this definition.
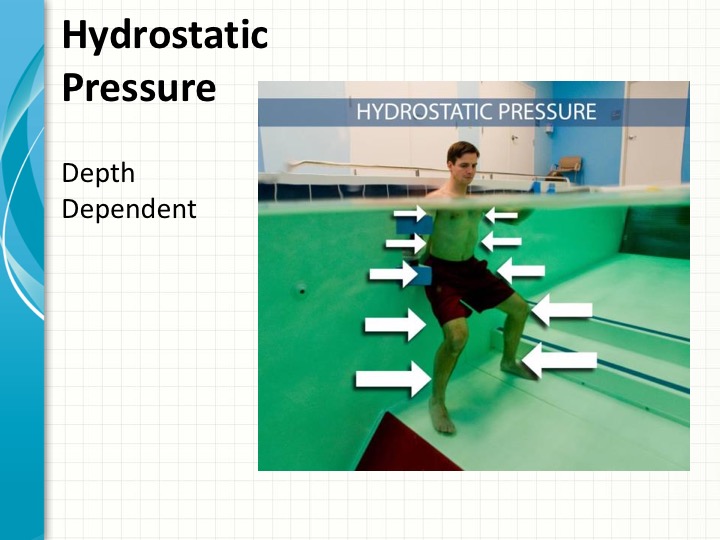
Figure 2. Overview of hydrostatic pressure.
His shoulders and chest are not submerged as far down as his feet, therefore they have less hydrostatic pressure. His feet are submerged deeper in the water that his waist, so therefore there is more pressure being exerted on them. His feet have a higher hydrostatic pressure than his waist. Pascal's law states that at any given depth the pressure from a liquid is exerted equally on all surfaces of the immersed object. A great effect of hydrostatic pressure is that it creates 3D pressure, meaning that the force comes at it from all directions. This plays a key role in aquatic therapy due to the support the hydrostatic pressure provides to all surface areas of a submerged body part. With this support, the hydrostatic pressure prevents the distal pooling, which will also assist in edema reduction. We need to consider this as we are submerging our patients into deeper water. Some pools you can adjust the depth of the water or you could go into the deep end of the pool, but before you submerge your patient, consider the depth of water and what impact this has on their body. This is very important to understand and keep this in mind as we later review the major systems of the body, and how immersion impacts them.
Viscosity
Figure 3. Overview of viscosity.
According to Wikipedia, the viscosity of a fluid is a measure of its resistance to gradual deformation by shear or tensile stress. For liquids, it corresponds to the informal concept of thickness. For example, honey has a much higher viscosity than water. Viscosity can be viewed in two ways. Kinetic viscosity is defined by the lubricants resistance to flow and shear due to gravity. To illustrate, imaging pouring two containers, one filled with water and one with honey. The rate at which each fluid flows is governed by its kinematic viscosity. Since the kinematic viscosity of water is lower, it flows faster. Dynamic, or absolute viscosity, is defined as the lubricant's resistance to flow as indicated by its measured resistance, best thought of as the amount of energy required to move an object. For example, consider placing a heavy metal rod in water versus in honey. It takes less energy to stir water compared to honey, because of the dynamic viscosity of water is lower. Viscosity is a physical property of fluids. It shows resistance to flow. Water has a low viscosity as it is thin.
Let's consider our aquatic therapy environment and how this impacts our patients. What affect does the viscosity have on their body as they move in the water? What about as they stand still in the water? Picture moving your body through a pool of water versus a pool of syrup. Which is harder? What impact does this have on your body and its systems? Viscosity provides our patients the most common form of resistance training. The water's viscosity allows for strengthening without the use of any equipment, and this resistance can be quickly altered by increasing the surface area. You can increase the surface area by giving them a piece of equipment to use. Using the water's resistance and the water's buoyancy, you can begin strengthening while decreasing the stress to the body.
I will use the term drag later in the presentation. Drag is the force caused by the water's viscosity and turbulence. You can also increase resistance by changing the speed of the movement in the water. The faster an object moves through the water, the greater the drag. The greater the drag, the greater resistance to movement, and the greater resistance, the greater muscle recruitment and contraction.
Specific Heat
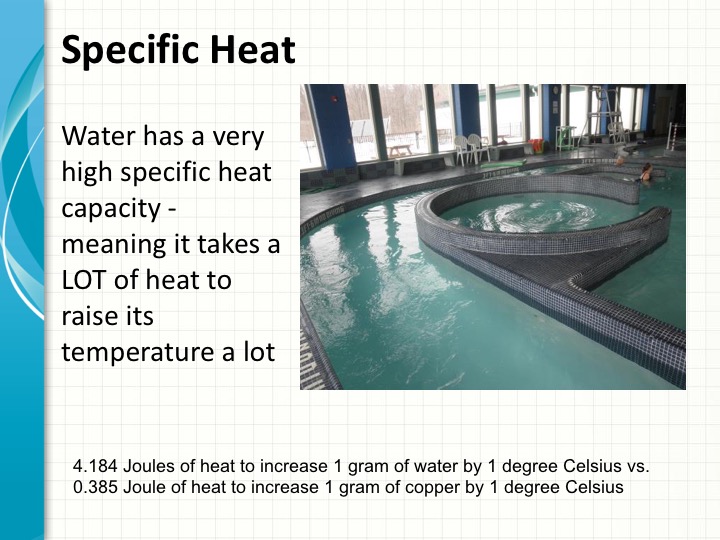
Figure 4. Overview of specific heat.
The amount of heat needed to increase the temperature of one gram of a substance by one degree is the specific heat capacity. It is expressed in Joules per gram per degree Celsius. According to the Department of the U.S. Interior, water does indeed have a high specific heat capacity. The specific heat of water is the amount of heat needed to raise its temperature a certain amount. One of water's most significant properties is that it takes a lot of heat to make it get hot. In fact, water has to absorb 4.184 Joules of heat for the temperature of one gram of water to increase by one degree Celsius. For comparison's sake, it only takes less than a half of one Joule to heat one gram of copper one degree Celsius. To understand this concept, think a bucket of water outside in the sun on a hot summer day. It will certainly get hot, but not enough to boil. However, if you walk barefoot on the black asphalt on that same hot summer day, you will likely burn your feet. Metals have a much lower specific heat capacity than water.
The fact that water has a high specific heat does play a role in aquatic therapy. We want to maintain our pools at a certain therapeutic temperature for our patients. If the pool is too cold, it will impact our patients in a very different way than if the water is too warm. It is going to be important to regulate your pool temperature. It is also important to take a daily record of the pool temperature to ensure that your patients are getting the most ideal therapeutic water temperature. Research says that the best temperature for aquatic therapy is 91 to 95 degrees Fahrenheit. To give you some perspective of that temperature, your typical YMCA lap pool is around 84 degrees. I have found that some patients cannot tolerate that high end of that range, especially those patients that have sports injuries or are working harder in the pool. I have found our typical patients perform best right around 92 degrees Fahrenheit. The warmer water increases their blood flow, muscle metabolism, and respiratory and cardiac rates. It also promotes relaxation and joint and muscle comfort. I recommend that you find a good temperature for your patients, and then try to regulate your pool to stay consistent with that same temperature. It always surprises me how patients will complain when our pool is at 90 or 91 degrees. They can tell the difference by just one or two degrees.
Refraction
Refraction is described in Webster's Dictionary as light or radio waves being deflected in passing obliquely through the interface between one medium and another, or through a medium of varying density. You can see, based on this photograph in Figure 5 that looking down into the pool at a patient's body submerged will look distorted. This is due to refraction.
Figure 5. Refraction example.
As you look at the picture on the upper left hand corner of Figure 6, in this case a pencil immersed in water looks bent due to refraction.
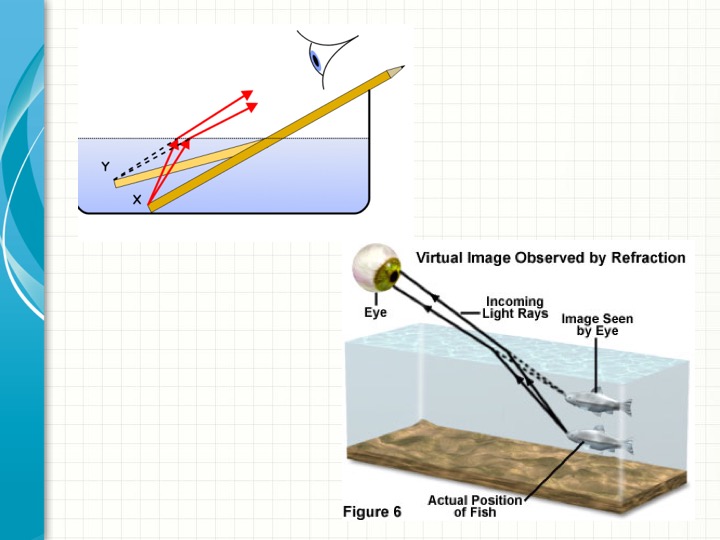
Figure 6. Overview of refraction.
The light waves from X change directions and seem to originate at Y. The electromatic waves constituting light are refracted when crossing the boundary from one transparent medium to another because of their change in speed. That is what makes this straight pencil appear bent. Although light waves can easily pass through materials like glass or water, the waves slow down as they travel through these materials. When the light waves slow down as they pass from one material to another, that is when they are going through refraction. When the light passes from air into a material like water, it slows down and always bends towards a line drawn perpendicular to the surface of the material. That is known as the normal line. When light passes from air into water, it bends toward this normal line. This explains why objects that you see under water are never where they appear to be. Your eyes cannot tell that the light is coming in a straight line so you see an image of the object that is in a different place than the real thing.
Refraction does play a role in aquatic therapy. It is often challenging for you to see what your patients are doing under water if you are looking down at them from the surface of the deck around the pool. This impacts patients as well. If you ask them to look down at their feet when they are doing a balance exercise, they are not going to get a correct representation as they would on land.
High tech pools today incorporate underwater cameras with a viewing screen above so that you and your patient can see what is really happening under water. I have a clip here to show you how that happens.

Here you can see our patient is walking under water. This pool is equipped with both a side view and a front view camera. This can help you to cue your patient. The therapist in this example is behind the patient. She is able to look up at this TV screen and monitor how well her patient is actually walking. She can now incorporate both tactile cues at the patient's legs as well as verbal cues as she is watching the patient move. The underwater camera gives her a much clearer picture than it would if she was looking down at the water at her patient's legs.
In summary, the principles of water that we have reviewed today are buoyancy which is the force exerted on an object under water. This aids our bodies by giving us the feeling of weightlessness. It allows for flotation and reduces the affects of gravity on an injured or aching joint or muscle. Hydrostatic pressure has more pressure the deeper you go. It plays a key role in our circulatory and pulmonary systems. Hydrostatic pressure supports and stabilizes the patient, allowing those with balance deficits to perform exercises without a fear of falling and decreasing their pain. Viscosity is a measure of resistance, and we learned water has a low resistance. We can change the resistance of water if we use jets or any other method to propel the water and create resistance. The greater the drag, the greater the muscle recruitment needed. Water's natural viscosity can be used to increase the rehabilitation process.
