Learning Outcomes
After this course, participants will be able to:
- Identify the central role of debriefing in the simulation learning process.
- Explain the three core principles of effective debriefing as they relate to adult learning theory.
- Identify two debriefing methodologies.
Practical Approaches for Engaging Simulation Learners
I appreciate your interest in exploring best practices for simulation debriefing. I am very passionate about the debriefing process and look forward to discussing it with you. In my role at Simucase, I work directly with graduate programs and provide clinical supervision to students across the nation. This experience has given me a deep appreciation—and a few hard-won lessons—about what truly turns a simulation into durable, real-world learning.
I wanted to share practical tips about how to make the most out of your debrief sessions. Running a great simulation is only half the battle. The real challenge is ensuring that simulated learning experience translates into sound judgment and behavioral change when your students face their next client.
In our course today, we will review research on why debriefing is the engine of learning, break down a practical “Debriefing Toolbox,” and explore specific, easy-to-implement methodologies such as Plus-Delta and Advocacy-Inquiry to keep your learners engaged, even over Zoom. While Simucase is used to reference case studies, the strategies discussed are fully applicable to any simulation format, whether virtual or in person, in a classroom or a dedicated lab.
When Does the Most Learning Occur During a Simulation Experience?
When does the most learning occur during a simulation experience? You might assume it happens during pre-work preparation or while students are immersed in the scenario itself. However, evidence tells a different story: the majority of learning occurs after the simulation—during structured debriefing. The simulation itself is essential because it creates an immersive experience and sets the stage for meaningful learning. But it's the post-event where structured reflection transforms experience into expertise, helping students develop both clinical skills and sound judgment.
Evidence for Simulation Debriefing and Clinical Reasoning in Physical Therapy
Physical therapy education research supports the idea that learning in simulation is strengthened when the simulated encounter is paired with a structured, reflective debrief. In a randomized controlled trial focused on physiotherapy students’ clinical decisions during a simulated low back pain (LBP) encounter, Sandoval-Cuellar et al. (2021) implemented simulation activities that included a structured debrief designed to promote reflection on clinical reasoning and decision-making. Both standardized patient and role-play formats were associated with improvements in decision-making skills related to LBP care, and the authors highlighted simulation paired with reflective discussion as a valuable pedagogic strategy in physiotherapy education (Sandoval-Cuellar et al., 2021).
In a repeated-measures study of DPT students participating in an 8‑week patient care management simulation course, Bizama and colleagues (2022) reported significant increases in students’ perceived clinical skills and clinical decision-making skills across time points spanning pre-simulation, post-simulation, and post–first clinical experience. The course design explicitly incorporated prebriefing, immersive simulation encounters, and structured debriefing as core components of each lab, with students reporting that the integrated simulation and debrief experiences helped them feel better prepared to enter their first clinical rotations (Bizama et al., 2022).
Together, these findings support the central premise of this course: simulation creates the experience, but debriefing provides the structured reflection that helps learners translate that experience into transferable clinical reasoning for future patient care (Bizama et al., 2022; Sandoval-Cuellar et al., 2021).
Contemporary Evidence for Simulation and Debriefing in Physical Therapy
Building on this foundation, newer studies continue to show that when physical therapy learners engage in realistic simulations followed by structured debriefing—whether in-person, computer-based, or telesimulation—they demonstrate meaningful growth in perceived competence, clinical decision-making, and sophistication of reasoning.
For example, Romano and Pasquale (2023) explored clinical reasoning strategies used by DPT students during a computer-based simulation followed by a structured written self-debrief. Students across three class years demonstrated increasingly sophisticated reasoning strategies, but the quality of self-reflection was highly variable, with no clear relationship between depth of reflection and the reasoning strategy used. The authors concluded that while simulation can elicit complex reasoning, learners often require explicit scaffolding and feedback during debrief to maximize the value of their reflective work (Romano & Pasquale, 2023).
Internationally, Westermeier et al. (2024) described the implementation of telesimulation and later in-person clinical simulation experiences for undergraduate physiotherapy students at a Chilean university. Across two semesters, students completed multiple scenarios emphasizing a comprehensive, person-centered approach to physiotherapy care. The authors noted that simulation provided a safe, structured environment for practicing clinical reasoning, and that debriefing—whether conducted virtually or in a dedicated simulation space—was critical for integrating patient context, function/health, and dysfunction/disease perspectives into learners’ decision-making (Westermeier et al., 2024).
Other contemporary studies further support the use of simulation as a vehicle for developing clinical reasoning when combined with opportunities for analysis and feedback. Torres and colleagues (2022) reported that interactive virtual musculoskeletal scenarios improved the clinical reasoning skills of undergraduate physiotherapy students, underscoring the utility of technology-enhanced simulation tools for repeated practice and reflection (Torres et al., 2022). A systematic review by Brentnall, Thackray, and Judd (2022) examined the evaluation of student health professionals’ clinical reasoning across placement and simulation settings, highlighting that simulation-based activities commonly incorporate post-scenario reflection or debrief as a mechanism to reveal and strengthen learners’ reasoning processes (Brentnall et al., 2022).
Taken together, these newer findings support and extend earlier work: when physical therapy learners encounter realistic, well-designed simulations and then engage in structured debriefing—whether via facilitator-guided dialogue, written self-debriefing, or mixed methods—they demonstrate meaningful growth in perceived competence, clinical decision-making, and the sophistication of their reasoning. In other words, contemporary research continues to affirm that in physical therapy education, simulation creates the experience, but debriefing is where learners consolidate meaning, confront reasoning gaps, and plan for future patient care.
These findings fit well with established learning theory frameworks that explain why reflection after an experience is so powerful—particularly when it is structured and facilitated.
Why Reflection is Key
Kolb's Experiential Learning Cycle: Learning is a cycle where concrete experience is followed by reflection, which leads to conceptualization and application. Without this deliberate space to reflect, the experience rarely crystallizes into durable behavioral change.
Research Consensus: Scholars such as Fanning and Gaba (2007) argue that the experience itself isn't learning; rather, it is the sense-making that follows the experience that deepens understanding.
Standard of Best Practice: In 2021, the INACSL (International Nursing Association for Clinical Simulation and Learning) affirmed that debriefing is not optional—it is the expected standard and the central driver of high-quality simulation education.
Debrief is the engine of learning in simulation. It takes the raw, intense experience and translates it into transferable knowledge and skill.
Adult Learning Theory in Debrief
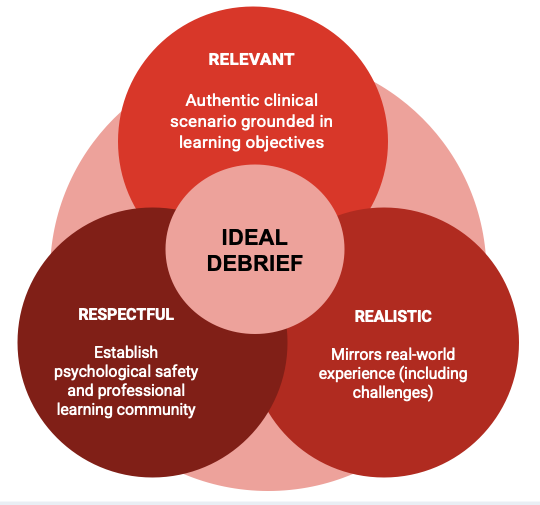
Figure 1. Adult learning Theory in Debrief.
When considering what should occur during a debrief, we draw on the principles of adult learning theory. Three essential elements guide this process: relevance, realism, and respect. Together, these create the foundation for meaningful learning and professional growth.
- Relevance: Knowles reminds us that adults engage most effectively with learning when it clearly connects to their needs, goals, and prior experiences. In a debrief, this means intentionally linking the stated learning objectives to the clinical decisions participants faced in the simulation.
- Realism: Both Kolb’s and Jeffries’ frameworks emphasize the value of authentic, practice-based experiences. The simulation should reflect real-world challenges, and the debrief should focus on applying new understanding in future clinical situations. This bridge between simulation and actual practice is where deep, lasting learning occurs.
- Respect: Respect serves as the foundation for psychological safety. A respectful environment allows learners to engage in honest self-assessment and reflection. Facilitators promote this by establishing clear norms, assuming positive intent, and using advocacy–inquiry techniques.
The INACSL Standards integrate these principles, emphasizing that effective debriefs connect to objectives, honor the learner, and feel authentic to real-world practice.
Applying Adult Learning Theory to Debriefing in Physical Therapy Education
Recent studies in physical therapy and broader health professions education reinforce that the principles of relevance, realism, and respect are not just theoretical ideals but practical design requirements for effective debriefing.
From a relevance standpoint, physical therapy learners consistently report that simulation-based learning is most impactful when scenarios and debrief questions are clearly tied to the clinical challenges they anticipate encountering in acute care, outpatient, community, or school-based settings. Bizama et al. (2022) showed that when DPT students participated in a simulation course explicitly linked to the patient-client management model, they reported significant gains in perceived clinical decision-making; debrief sessions guided students to connect each simulated decision back to core evaluative and intervention processes used in real practice (Bizama et al., 2022). Similarly, in the randomized trial by Sandoval-Cuellar et al. (2021), debriefing conversations focused directly on the clinical decisions made during low back pain encounters, including guideline-consistent management and communication with people experiencing pain. These targeted debriefs helped learners see how evidence-based decision-making translated into specific actions during the simulation and, importantly, could be generalized to future patients (Sandoval-Cuellar et al., 2021).
Realism in debrief is supported not only by high-fidelity manikins or standardized patients but also by the authenticity of the reasoning tasks. Romano and Pasquale (2023) demonstrated that even in screen-based simulation, asking DPT students to articulate how they prioritized impairments, interpreted patient responses, and selected interventions prompted them to use more advanced reasoning strategies, particularly in later years of training (Romano & Pasquale, 2023). In the telesimulation work described by Westermeier et al. (2024), facilitators designed debrief prompts that required students to integrate functional outcomes, environmental context, and patient goals—elements that mirror real-world complexity in physiotherapy decision-making (Westermeier et al., 2024). When debrief questions are grounded in realistic, multi-factorial clinical problems rather than abstract content review, learners are more likely to internalize and transfer their learning.
Respect and psychological safety also emerge as non-negotiable conditions across contemporary simulation research. High-fidelity simulation studies in nursing, for example, consistently describe prebriefing and debriefing as opportunities to reduce anticipatory anxiety, promote honest discussion of errors, and frame mistakes as learning data rather than personal failures (El Hussein et al., 2023). Physical therapy students in simulation courses similarly report that feeling supported by faculty, being given permission to make and analyze errors, and engaging in debriefs where all voices are invited enhances their willingness to share their reasoning, ask questions, and critically examine their own performance (Bizama et al., 2022; Romano & Pasquale, 2023).
When physical therapy educators intentionally design debriefs that (1) clearly connect to stated learning objectives and practice expectations (relevance), (2) require learners to grapple with realistic, context-rich clinical decisions (realism), and (3) are conducted in a climate of psychological safety and mutual respect (respect), they operationalize adult learning theory in a way that reliably supports clinical reasoning and professional identity formation.
Debriefing Toolbox
- “Just right” prebrief
- Language to establish psychological safety
- Pick a debrief method
- Anchor in objectives
- End with transfer
I would like to share a few ideas related to what I call a debriefing toolbox. When we think about what we expect from a debrief, our goal is always to set students up for success. That process begins well before the simulation itself—with the pre-brief.
Before starting a simulation, we want to provide learners with what I like to call a “just-right” pre-brief. This means offering the right amount of information and support to prepare them for the learning experience ahead—enough to orient them and reduce anxiety, but not so much that it limits discovery. In my experience, the stronger and more thoughtful your pre-brief, the more effective your debrief will be because a well-prepared learner is better able to reflect, engage, and grow during debriefing.
Once the simulation is complete and we transition into the debrief, keep several essential principles in mind. The first is to set the stage for success by establishing psychological safety. Learners will not open up if they feel judged, shamed, or unsafe. Establish ground rules at the beginning of the debrief by reminding students that this is a learning space, that mistakes are both expected and valuable, and that feedback is meant to foster growth rather than punishment. When I debrief students, I often tell them, “We are here to learn together—it is okay not to be perfect.” Simple phrases like that go a long way in reducing anxiety and encouraging honest reflection, especially when discussing moments that didn’t go as planned.
The next key step is to choose a debriefing method. There isn't one “perfect” or universal approach. The best method depends on your learners’ level, the complexity of the simulation, and the session’s goals. What matters most is intentionality—selecting a structured approach and committing to it, rather than improvising. A consistent framework helps guide the discussion and ensures learners get the most out of the experience.
Third, it is essential to anchor the conversation in your learning objectives. It is easy for discussions to drift into unrelated stories or side topics during debriefs. When that happens, gently bring the conversation back to the stated objectives. I often remind students what I hope they will take away from the experience to keep the focus clear and purposeful.
Finally, we always want to end with a transfer. This is where the true power of debriefing lies—helping learners connect what they have learned to real-world practice. Ask questions like, “How will you apply what we discussed today to your next client—or even to a client you haven’t met yet?” When learners articulate the “so what” of their experience, they bridge the gap between simulation and clinical practice.
To summarize: start safe, pick your method, anchor in objectives, and finish strong with transfer to practice. When these elements come together, debriefing becomes not just a review of what happened, but a transformative learning experience that prepares students to think critically and act confidently in the real world.
Goldilocks Principle of Prebriefing
Prebriefing, a key debriefing tool, should follow the Goldilocks principle: providing just the right amount of support before simulation-based learning. Too little support increases anxiety and guesswork, while too much risks spoon-feeding and dulling the experience. The prebrief must be calibrated to the learner, considering four key areas.
- Academic experiences: What coursework have they completed? Understanding this helps us gauge their foundational knowledge.
- Clinical experience: What have they actually done in practice and at what level of independence? This helps us tailor scenarios and discussions to their skill level.
- Background knowledge: Are there prerequisite concepts, protocols, or procedures we need to review to ensure learners have the necessary knowledge to succeed in the simulation?
- Previous simulation experience: Have learners participated in simulations before? Do they understand the debriefing roles, norms, and expectations?
By asking these questions, we can ensure the prebrief orients learners without removing the challenge and opportunity for independent learning that makes simulation so powerful.
Same Case, Very Different Prebriefs…
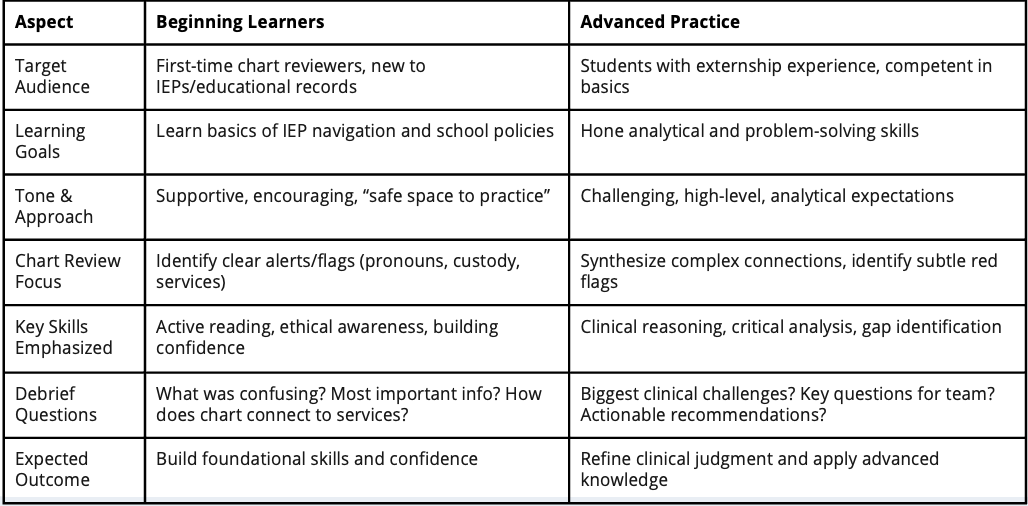
Figure 2. Beginning Learners and Advanced Practice.
To modify the prebrief to meet learners' needs, let's consider a simulation using the Electronic Documentation School Setting Part Task Trainer from Simucase, where students review school documentation. This case is interdisciplinary, but I will show two different prebrief approaches for the same case, tailored to the learners' experience. Refer to Figure 2.
If I were prebriefing a group of beginning learners—for example, first-semester graduate students who have little hands-on experience in schools—I might say something like this:
"Next week, we’ll work with the Electronic Documentation School-Setting Part Task Trainer. In this case, you’ll have the opportunity to review an educational record and explore an IEP in a safe and supportive environment. The focus should be on learning, not perfection, so approach this as a chance to build your skills and confidence as you navigate these documents. You’ll be reviewing the IEP for Kai, a 12-year-old student with complex medical needs. Pay close attention to the details, including the services they are receiving, custodial considerations, and pronoun use. As you work through the case, focus on being an active reader: treat the record like a puzzle and notice any alerts or flags that might impact Kai’s educational experience. Keep ethical and legal principles, like privacy and confidentiality, in mind throughout.
At debrief, be prepared to reflect on what you found challenging, the most impactful pieces of information in the educational record, and how the IEP connects to Kai’s overall educational journey. Remember, this is about practice and growth—dive in and do your best."
On the other hand, if I’m assigning this simulation to students who are further along in their academic journey—perhaps they have had placements in schools or worked with school-age clients—the pre-brief would look different. For this group, I might say something like:
"Next week, you’ll be completing the Electronic Documentation School-Setting Part Task Trainer simulation, building on your previous externship experience. I want you to think about how this simulation will challenge your clinical reasoning and problem-solving skills beyond a basic document review. Focus on synthesizing how Kai’s diagnosis, educational history, and services all connect. Be attentive to underlying issues or red flags that could impact an IEP meeting as the team works together.
Analyze the IEP goals and interventions to determine whether they align with Kai’s needs, and look for potential gaps in services. In the debrief, be prepared to discuss the most significant clinical challenges, the questions you would pose to Kai’s team to gain deeper insight, and concrete, actionable recommendations to strengthen support for them. This is your opportunity to sharpen your clinical judgment using a real-world scenario."
This example illustrates how the pre-brief should vary based on learner level, even for the same case. For beginners, the focus is on orientation, foundational skills, and confidence-building. For more advanced learners, the emphasis shifts to critical thinking, synthesis, and clinical decision-making.
Establishing Psychological Safety
The next critical element of effective simulation is establishing psychological safety—the foundation of meaningful debriefing and team learning.
When learners feel safe, they are more likely to speak up. They share honest feedback, admit mistakes, and ask questions without fear of judgment. This shift from blame to understanding enables us to examine the root causes and learn from errors rather than hiding them.
When we provide a genuinely safe environment for students to process what happened, we help them reset emotionally. This matters because we know that safety must come first—learning follows naturally once students feel secure enough to engage fully in reflection.
Establish Safety and Revisit Norms Often!
I am sharing some of the language I use in my debrief groups to help establish psychological safety, as shown in Figure 3.
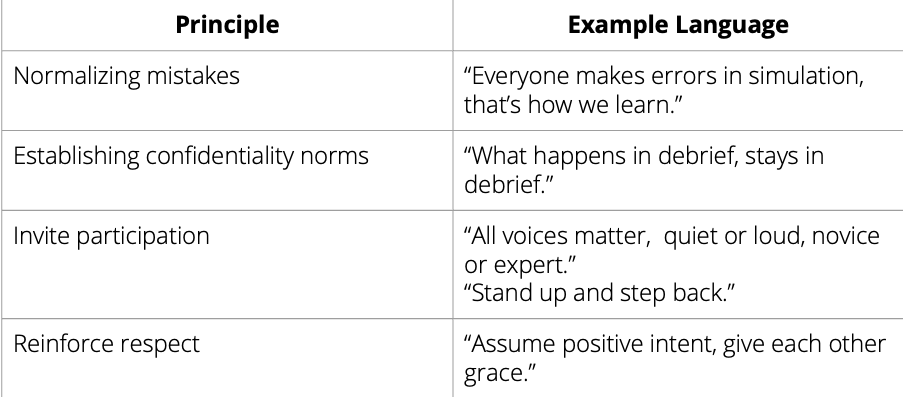
Figure 3. Example Language chart.
I would like to share some of the language I frequently use in my debrief groups to help establish psychological safety (see Figure 3). To promote psychological safety in debriefs, I normalize mistakes by explaining that errors are expected in simulation and are essential for learning, both individually and collectively.
Another important component is establishing confidentiality norms. I often say, “At the risk of sounding cheesy, what happens in debrief stays in debrief.” This helps create a privileged learning space where everyone knows that conversations are private and respected.
I also prioritize inviting participation from all learners, including those who may be quieter. I tell students that all voices matter—loud or quiet, novice or expert—and that we want to hear everyone’s reflections. One of our supervision team members often uses the phrase, “Stand up and step back.” That is, speak your perspective, then step back to allow space for others to contribute.
Finally, we reinforce respect and positive intent, especially if discussions become tense. I often remind students, “We assume positive intent and work together. We give each other grace.”
By introducing these psychological safety cues at the start of debrief and circling back to them as needed, we create a focused, respectful, and open environment. This enables learners to engage in honest reflection and delve deeply into the simulation's content, ultimately supporting meaningful learning and growth.
Common Debriefing Methodologies
In this section, I will describe several commonly used debriefing approaches and show how they can fit into a simple, four-step structure for debriefing a physical therapy simulation. Rather than thinking of the methods as separate or competing, it can be helpful to see them as tools you can use at different points in a debrief.
A practical way to structure most 20–40‑minute debriefs is to move through four broad phases:
- Settle and Normalize – Check in emotionally and re-establish psychological safety.
- Reconstruct the Story – Build a Shared Understanding of What Happened.
- Analyze Clinical Reasoning – Dig into how and why decisions were made.
- Consolidate and Transfer – Summarize key takeaways and link them to future practice.
The debriefing methodologies discussed in this section can be applied within one or more of these phases.
Step 1: Settle and Normalize (2–5 minutes)
- Begin with a brief emotional “check-in,” especially after high-stakes or emotionally charged simulations (e.g., rapid functional decline, complex family interactions, or adverse events).
- Ask open questions such as, “What’s one word that captures how you’re feeling right now?” or “What stood out for you emotionally during the scenario?”
- Normalize anxiety and imperfection, reminding students that simulation is a protected learning space where errors are expected and valuable. Evidence from both nursing and DPT simulation suggests that this early normalization reduces performance anxiety and increases engagement in later reasoning-focused discussion (Bizama et al., 2022; El Hussein et al., 2023).
Step 2: Reconstruct the Story (5–10 minutes)
- Invite learners to briefly reconstruct what happened: “Walk me through the encounter from your perspective. What did you notice first? What decisions did you make, and when?”
- Encourage multiple voices so the group gains a shared mental model of the case.
- This “gather” phase parallels the first step of the GAS approach and supports learners in organizing their experiences before analyzing them (Fanning & Gaba, 2007).
Step 3: Analyze Clinical Reasoning (10–20 minutes)
- Use your chosen debrief method, which we will talk about soon. (Plus-Delta, GAS, Advocacy–Inquiry, or a combination) to explore how and why learners made particular decisions.
- For example, in a neurorehabilitation simulation, you might say: “I noticed that you prioritized gait training early in the session, even though the patient reported significant fatigue. I’m curious about how you weighed endurance, safety, and patient goals when you made that choice—can you share your thinking?”
- Studies of physical therapy students’ reasoning in simulation indicate that asking learners to describe how they identified key impairments, interpreted patient responses, and adjusted their plan helps surface novice versus more expert-like patterns of reasoning (Romano & Pasquale, 2023; Torres et al., 2022).
- Where possible, bring in brief evidence-based touchpoints—clinical practice guidelines, outcome measure cut-scores, or current best evidence—to model integration of research, clinical expertise, and patient values.
Step 4: Consolidate and Transfer (5–10 minutes)
- End by explicitly connecting insights from the simulation to real-world physical therapy practice.
- Ask questions such as:
- “How will this experience change the way you approach a similar patient on your next clinical rotation?”
- “What is one specific behavior you want to try in your next lab, simulation, or clinical day?”
- Research on simulation-based learning across health professions shows that when learners articulate concrete “next steps,” they are more likely to enact behavior change and report greater confidence during early clinical experiences (Bizama et al., 2022; Westermeier et al., 2024).
Across all four steps, the facilitator’s stance is crucial. Studies of faculty development in simulation emphasize that effective debriefers consistently demonstrate curiosity, humility, and a coaching mindset rather than a judging stance (Cheng et al., 2015). In physical therapy education, this might involve openly acknowledging the complexity of decisions surrounding prognosis, intervention dosage, or discharge planning, and modeling how experienced clinicians think aloud, consult evidence, and solicit team input when faced with uncertainty.
By intentionally structuring debriefs in this way, physical therapy educators can better ensure that each simulation moves beyond “what happened” toward the deeper questions of “why did it happen?” and “how will I respond differently next time?”—the core drivers of clinical reasoning growth.
Next, I would like to spend a little time discussing common debrief methodologies, which can be applied to any simulation—not just Simucase.
Plus Delta Debriefing
One of my favorite approaches is the Plus-Delta debriefing method. In Plus-Delta, we divide the discussion into two parts: the Plus, where we focus on what went well, and the Delta, where we focus on areas for change or improvement.
Plus-Delta is especially useful in Step 3 (Analyze Clinical Reasoning) and Step 4 (Consolidate and Transfer) of the framework above. After you reconstruct the story together, you might say:
- “Let’s start with the Plus. What are specific things you did in this encounter that you would want to repeat with a similar patient?”
- “Now let’s move to the Delta. What is one thing you would change next time, and what will that look like in practice?”
On the Plus side, we highlight strengths and effective behaviors. This isn't just "fluff"—it makes good practices visible so learners can repeat them. For example, if a learner were completing a pediatric physical therapy assessment case, they might say:
"I did really well when collecting my patient’s case history. When I came across her rare neuromuscular diagnosis, I wasn’t sure what it was, so I researched it and how it affects her strength, endurance, and motor development. This helped me address the family’s concerns effectively and tailor my assessment to her functional needs."
This is a concrete success we want to reinforce and carry forward.
Next, we move to the Delta side—the improvement column. Here, the focus is on identifying something that didn’t go as planned and turning it into a clear, actionable step. For instance, a learner might reflect:
"I had difficulty selecting and scoring the appropriate gross motor outcome measure because I rushed and used the wrong age-normed section, which led to an inaccurate interpretation of the results. Next time, I will slow down, double-check the administration guidelines, and verify that I’m using the correct age band and scoring instructions before interpreting the scores."
Notice the structure: a specific gap is identified, along with a corresponding action step to address it.
There are two key rules that make Plus-Delta work effectively:
- Start with the Plus: Highlighting strengths first creates a positive, supportive environment. Learners respond better when we acknowledge what they did well before discussing areas for improvement.
- Make Deltas actionable: Any area for improvement should include a concrete next step—what exactly will the learner do differently in the future?
Used consistently, Plus-Delta helps teams celebrate successes, identify areas for growth, and create a clear roadmap for improvement. It also promotes a positive, non-judgmental environment and encourages honest, constructive feedback during debrief sessions.
Gather - Analyze - Summarize (GAS) Approach
Another debrief approach I commonly use is called the GAS approach, which stands for Gather, Analyze, Summarize.
The GAS approach aligns closely with the four-step structure:
- The Gather phase overlaps with Step 2 (Reconstruct the Story) as you invite learners to describe what they saw, thought, and felt during the simulation. This involves exploring the learner’s feelings, perceptions, and observations of what actually happened during the simulation. The goal is for learners to feel heard while reinforcing respect and fostering a sense of psychological safety. It also gives the facilitator insight into how learners interpreted the scenario.
- The Analyze phase is essentially Step 3 (Analyze Clinical Reasoning), here learners engage in reflection and critical thinking, considering why they made certain decisions and exploring alternative approaches. This step aligns closely with Kolb’s reflective observation and abstract conceptualization phases, allowing learners to deepen their understanding of the experience.
- The Summarize phase maps directly onto Step 4 (Consolidate and Transfer), where you identify key learning points and link them to future patients, supporting transfer of knowledge to future clinical scenarios.
In practice, you might say:
- “Let’s start by gathering: what happened from your perspective?”
- “Now let’s analyze: why did you choose that test, or that intervention, at that moment?”
- “To summarize, what are your top two takeaways, and how will they shape your next similar encounter?”
The GAS approach is simple, structured, adaptable, and promotes meaningful reflection. Its three-step framework makes it an excellent, easily implementable method for facilitators new to simulation-based learning.
Advocacy - Inquiry Method
Another approach you can use to debrief simulations is the Advocacy-Inquiry method. With advocacy, we clearly identify and describe our observations, and then move into inquiry, where we explore the learner’s reasoning.
Advocacy-Inquiry can be woven into Step 3 (Analyze Clinical Reasoning) whenever you want to surface the thinking behind a particular action.
For the advocacy step, you focus on specific observations and share your interpretation using “I” statements. Because we often review simulations after they have occurred, we can gather this information from learner transcripts.
For example, using a pediatric gait assessment case in physical therapy, I might say:
"I observed that several of you had difficulty differentiating the primary contributors to your patient’s gait deviations. Many of you focused mainly on the foot position and seemed unsure whether the primary issue was related to decreased proximal stability, joint range of motion, or abnormal tone. I am concerned we might be conflating overlapping features and not clearly prioritizing the main impairment driving the gait pattern."
The key here is to be specific and objective while avoiding labeling any learner as right or wrong. This establishes a neutral and constructive tone for discussion.
Next comes inquiry, where we express genuine curiosity about the learner’s thought process. For instance:
"I’m wondering what your reasoning was as you weighed these possible contributing factors. What cues in this case guided you one way or another—for example, observations from the video, results from strength or range of motion testing, or the child’s fatigue level? Can you help me understand which information or evidence felt most persuasive?"
The goal of inquiry is to surface assumptions and decision-making processes in an open and non-judgmental manner. This approach reveals clinical reasoning and creates conditions for self-correction, helping learners reflect on their decisions and improve future performance.
Evidence-Informed Use of Plus–Delta, GAS, and Advocacy–Inquiry in Physical Therapy Simulation
Although Plus–Delta, GAS, and Advocacy–Inquiry were originally described in broader simulation and crisis resource management contexts, emerging evidence suggests they can be thoughtfully adapted to the needs of physical therapy learners and curricula.
Plus–Delta in Physical Therapy Contexts
In simulation courses where DPT students repeatedly encounter varied patient populations (e.g., cardiopulmonary, neurorehabilitation, outpatient orthopedics), Plus–Delta can be used to scaffold increasingly sophisticated self-assessment. Early in the curriculum, “Plus” items may center on foundational skills such as patient safety behaviors, basic communication, and completion of required examination components. As students progress, the “Plus” column can explicitly target more advanced reasoning behaviors (e.g., hypothesis generation, prioritization of impairments, justification of outcome measures). The “Delta” column then becomes a place to document specific, actionable changes in reasoning or behavior tied directly to upcoming learning opportunities (future labs, simulations, or clinical days). Repeated use of this structure is consistent with simulation research showing that sequenced, reflection-rich experiences support growth in clinical decision-making and perceived readiness for practice (Bizama et al., 2022; Sandoval-Cuellar et al., 2021).
GAS Approach for Integrating Function and Context
The GAS framework is particularly helpful for highlighting the International Classification of Functioning, Disability, and Health (ICF) perspective that underpins contemporary physical therapy practice. During the “Gather” phase, facilitators can elicit not only what learners did but also what they noticed about the patient’s participation, environmental barriers, and personal factors. The “Analyze” step then becomes a natural space to discuss how those contextual elements informed (or should have informed) students’ choice of interventions, dosage, and education strategies. Finally, the “Summarize” phase can explicitly link key takeaways to ICF-based documentation, goal setting, and interprofessional communication. This kind of structured reflection is consistent with reports that simulation experiences, which emphasize context and function, help physiotherapy students develop more holistic clinical reasoning (Westermeier et al., 2024).
Advocacy–Inquiry to Reveal Clinical Reasoning Pathways
Advocacy–Inquiry is especially valuable in uncovering subtle reasoning errors that might not be visible when learners only report what they did, rather than why.
For example, in a gait analysis simulation, a facilitator might say, “I noticed that you quickly attributed the patient’s knee hyperextension to quadriceps weakness and moved on to strengthening exercises, and I’m concerned we may have underexplored contributions from spasticity or proprioceptive loss. Can you walk me through how you weighed those potential causes in your reasoning?”
By sharing an observation and concern and then inviting learners to unpack their thinking, the facilitator simultaneously offers feedback and honors the learner’s perspective. Romano and Pasquale’s (2023) findings that DPT students’ reasoning strategies vary in sophistication, even at more advanced stages of training, underscore the need for this kind of guided exploration; learners benefit from opportunities to “think aloud” about how they synthesized examination data, prioritized hypotheses, and selected interventions (Romano & Pasquale, 2023).
Across methods, the common thread is intentionality. The choice of Plus–Delta, GAS, Advocacy–Inquiry, or another structured approach should be driven by the simulation’s objectives, the learners’ developmental level, and the kinds of reasoning you most want to surface. Consistent with recent reviews of clinical reasoning assessment in simulation, clarity about what you are trying to elicit—pattern recognition, hypothesis testing, narrative reasoning, ethical deliberation—helps ensure that the debrief methodology you select truly supports the desired learning outcomes (Brentnall et al., 2022).
Tips from The Simucase Supervision Services Team
Next, I want to share some tips from the Simucase Supervision Team. Our team regularly leads debriefs for graduate students. I asked our supervisors: “If you were offering advice to a new faculty member just learning how to debrief, what would you share?” Here are some of their responses:
- Connect cases to real-life experience: Sharing anecdotal clinical experiences to help learners see how the case relates to real-world practice. This helps students understand the practical relevance of what they’re learning.
- Role-play communication: Learners can practice explaining their findings. For example, “How would you explain these results to the family? How would it change if you were presenting to a teacher?” This encourages learners to reflect on their language and communication strategies in various contexts.
- Manage tangents effectively: Another supervisor noted that discussions can easily go off track. To refocus, she often uses the “parking lot” approach: “That’s a great point—let’s put that in the parking lot and come back to it later.”
Embrace silence: One of the most important tips is to recognize the magic in silence. When a question is posed, resist the urge to immediately fill the space. Waiting 5 to 15 seconds can feel uncomfortable at first, but it gives learners time to think and reflect. Over time, you’ll see that this pause often leads to more thoughtful responses.
These tips, drawn from experienced supervisors, can help new faculty build confidence, structure discussions effectively, and foster meaningful reflection during debrief sessions.
I also asked our supervision team about their favorite debrief questions, and I wanted to share some of those with you. Again, these questions are great for debriefing Simucase content, but can also be applied to any simulation, whether completed in a lab or classroom. One of my personal favorites is:
"If you could go back in time and offer yourself advice—a fast rewind to a week ago—what would you tell yourself? What do you wish you had known before starting this simulation?"
Other questions shared by supervisors include:
"How might this experience change the way you approach a similar patient in the future?"
"How did the information you gathered in the case history section influence your assessment and treatment plan?"
"What surprised you or caught you off guard when you were working on this case?"
These questions often uncover hidden assumptions or gaps in understanding, providing valuable insight that can be addressed in the debrief discussion.
While these practical tips and debrief questions can immediately support individual faculty in leading more meaningful conversations with learners, their impact is magnified when they are embedded within a broader, program-level strategy. Rather than viewing each debrief as a standalone teaching moment, physical therapy programs can intentionally weave simulation and debriefing across the curriculum to systematically cultivate students’ clinical reasoning. This brings us to the next focus: program-level integration of simulation debriefing in DPT curricula.
Program-Level Integration of Simulation Debriefing in Physical Therapy Curricula
Program-level planning is essential to ensure that simulation and debriefing are not isolated experiences, but instead form a coherent thread that supports the development of clinical reasoning across the entire curriculum. Recent work in DPT education highlights several design considerations.
First, curricula that intentionally sequence simulation experiences from lower- to higher-complexity cases, with matched expectations for debrief participation, appear to support progressive refinement of reasoning. Bizama et al. (2022) described a course in which PT students engaged in multiple simulation-based learning activities across outpatient and community-based settings, each accompanied by faculty-led debriefing. Students’ perceived clinical skills and decision-making abilities improved significantly over time and were maintained into their first clinical experiences, suggesting that repeated cycles of simulation and debrief can help close the gap between classroom learning and clinical practice (Bizama et al., 2022).
Second, assessment and feedback practices should be aligned with the goals of debriefing. Romano and Pasquale (2023) found that while DPT students employed a range of clinical reasoning strategies during computer-based simulations, the quality of their written self-debriefing reflections varied widely (Romano & Pasquale, 2023). This suggests that programs may need to explicitly teach what high-quality reflection looks like and provide formative feedback on students’ debrief contributions, whether oral or written. In parallel, systematic reviews of clinical reasoning evaluation in simulation emphasize the importance of using validated tools and clearly defined constructs when assessing reasoning performance (Brentnall et al., 2022). When faculty align debrief questions, grading criteria, and feedback with these constructs, learners receive consistent messages about what constitutes “good reasoning.”
Third, physical therapy programs should prioritize faculty development, specifically for debriefing purposes. It is a common misconception that clinical expertise automatically translates to teaching effectiveness. Even highly experienced PT clinicians—who are experts at providing direct patient feedback—may struggle to facilitate a simulation debrief that balances psychological safety (where learners feel safe to make mistakes) with intellectual challenge (where learners are pushed to analyze their reasoning).
As emphasized by Cheng et al. (2015), effective simulation training must extend beyond the operational mechanics of 'running the manikin' or managing the equipment. Instead, development should focus on facilitation competencies: mastering specific debriefing structures (such as GAS or PEARLS), utilizing open-ended questioning techniques to uncover clinical reasoning, and managing complex group dynamics. When a PT program establishes this shared debriefing language, it ensures that learners encounter a consistent educational experience.
Finally, simulation and debriefing should be explicitly linked to program outcomes and accreditation expectations related to clinical reasoning, professional behaviors, and patient-centered care. As clinical reasoning is increasingly recognized as a core competency and a key focus of entry-level PT education, simulation-based learning that includes high-quality debriefing offers a powerful mechanism for demonstrating that graduates can not only perform technical skills but also justify and adapt their decisions in complex, uncertain environments. By documenting how simulation scenarios align with program learning outcomes and how debriefing is utilized to assess and support those outcomes, programs can provide a straightforward narrative of how they are preparing future physical therapists for safe, effective, and reflective practice.
Final Thoughts
Debriefing is a deliberate, structured process intended to foster reflection, critical thinking, and skill development by connecting theory to practice and identifying growth areas in a supportive environment.
High-quality debriefing starts with a prebrief that sets clear expectations and prepares learners. The debrief itself relies on psychological safety and structured methods (e.g., Plus-Delta, GAS, Advocacy-Inquiry) for meaningful dialogue, self-assessment, and collaborative learning. The four-step practical framework (Settle and Normalize, Reconstruct the Story, Analyze Clinical Reasoning, Consolidate and Transfer) provides a flexible yet structured guide for facilitators to integrate these methods effectively, ensuring a comprehensive and purposeful debriefing experience.
Engagement, especially in virtual settings, is vital. Varying methods, such as polls, breakout rooms, and role-playing, maintain attention and promote participation. Pacing, acknowledging strengths, and analyzing challenges enhance confidence and clinical reasoning.
Debriefing serves as a powerful model for professional behavior. When faculty demonstrate curiosity and respect, they help learners internalize these qualities, ultimately enhancing their communication and decision-making skills. These methodologies are not merely theoretical; they are supported by contemporary research in physical therapy and health professions education that confirms their effectiveness in fostering clinical reasoning and professional identity. Furthermore, encouraging learners to articulate their rationale helps surface knowledge gaps and strengthens the habits of lifelong learning.
Finally, for maximum impact, debriefing should not be an isolated event but strategically integrated into the curriculum at a program level. This involves thoughtful sequencing of simulation experiences, alignment of assessment, and ongoing faculty development to ensure consistency and continuous improvement in fostering clinical reasoning across the entire DPT program. Effective debriefing is iterative, flexible, responsive to group needs, and grounded in evidence. Thoughtfully integrating pre-briefing, engagement, structured methods, and supervision creates powerful, lasting impacts on clinical competence and professional growth.
Ultimately, debriefing is where real learning happens: reflection meets action, moving learners from observing to understanding and doing, and crucially, transforming raw experience into refined clinical reasoning and decision-making skills essential for competent physical therapy practice.
References
A complete reference list is provided in the course handout.
Citation
Ligon, E , Vela, F., and Kelly, C. (2025). Practical approaches for engaging simulation learners during simulation debriefing. PhysicalTherapy.com, Article 4980. Retrieved from https://PhysicalTherapy.com


