Editor's note: This text-based course is a transcript of the webinar, Interdisciplinary Approach To Stroke Rehabilitation: Outpatient, Home Health, And Community Rehabilitation Phase, presented by Alaena McCool, MS, OTR/L, CPAM, Katherine George, PT, DPT.
Learning Outcomes
- After this course, participants will be able to:
- Analyze the components that make up an effective home program for a client and caregiver.
- Evaluate 3 evidence-based interventions that OTs and PTs use in outpatient treatment based on the patient’s neurological symptoms.
- Recognize effective collaboration between OT and PT throughout the post-stroke inpatient phase via discussion of case studies.
Contents
- Disclosures
- Introduction
- Recap from Part 1
- Stroke Facts/Current Updates
- Case Study Reintroduction
- Home Health Rehabilitation
- Outpatient Rehabilitation
- Barriers
- Community Reintegration
- Literature Update
- Case Studies
- Questions and Answers
Katie: The first presentation focused on implementing interdisciplinary approaches to rehab in acute care and inpatient rehab settings. We are going to review some of the slides related to stroke definitions today in this presentation in case you were not able to attend.
Stroke Definitions
- Ischemic Stroke (87% of strokes)
- Obstruction in cerebral vasculature preventing brain tissue from getting oxygen and nutrients, causing cell death
- Hemorrhagic Stroke (13% of strokes)
- Blood vessel rupture or leakage causing blood to flow into brain tissue
Tsao, C. W., Aday, A. W., Almarzooq, Z. I., Alonso, A., Beaton, A. Z., Bittencourt, M. S., Boehme, A. K., Buxton, A. E., Carson, A. P., Commodore-Mensah, Y., Elkind, M. S. V., Evenson, K. R., Eze-Nliam, C., Ferguson, J. F., Generoso, G., Ho, J. E., Kalani, R., Khan, S. S., Kissela, B. M., … Martin, S. S. (2022). Heart disease and stroke statistics—2022 update: A report from the American Heart Association. Circulation, 145(8). https://doi.org/10.1161/cir.0000000000001052
Ischemic strokes are due to obstructions and vasculature preventing brain tissue from getting oxygen and nutrients. Hemorrhagic strokes are due to blood vessel rupture or leakage, which causes blood flow into the brain tissue, and, eventually, cell death. Eighty-seven percent of all strokes are ischemic, and about 13% are hemorrhagic. Hemorrhagic strokes tend to have worse outcomes, both medically and functionally.
Common Presentations
These are common presentations in this chart.
Middle Cerebral Artery | •Largest vessel branching from internal carotid artery •Supplying large areas of the frontal/temporal/ parietal lobes and basal ganglia | •Contralateral strength and sensory loss in face/arms > legs •Contralateral homonymous hemianopia •Aphasia with L sided MCA strokes •Neglect with R sided MCA strokes |
Anterior Cerebral Artery (ACA) | •Branching from internal carotid artery •Supplies portions of the frontal and parietal lobes | •Contralateral strength and sensory loss in legs > arms •Confusion, delayed response times, memory deficits •Apraxia possible |
Posterior Cerebral Artery (PCA) | •Branches from basilar artery •Supplies occipital and temporal lobes, thalamus | •Visual deficits •Contralateral strength and sensory loss •Aphasia with L PCA strokes •Neglect with R PCA strokes |
Vertebral Arteries/ Basilar Artery | •Vertebral arteries join to form basilar artery •Supplies posterior portion of brain, including cerebellum and brainstem | •Vertigo, visual deficits, and speech deficits, balance and coordination deficits, including ataxia with cerebellar strokes •Strength, sensation, vision, swallowing, breathing, and arousal deficits with brain stem strokes |
These are general overviews of what you may see on your caseload.
Stages of Stroke
- Hyperacute: 0-24 hours
- Acute: 1-7 days
- Early Subacute: 7 days-3 months
- Late Subacute: 4-6 months
- Chronic: 6 months+
Some more definitions here. We're going to be addressing the early subacute, late subacute, and chronic phases during today's presentation.
Stoke Quick Facts
- “Leading cause of serious long-term disability”
- Global Incidence: 11.71 million people
- United States Incidence: ~ 795,000 people
(Tsao et al., 2022)
Stroke is the leading cause of serious long-term disability. The incidence of strokes in the US and globally are very high. Additionally, one in four stroke survivors will have another stroke in their lifetime, and these recurrent strokes have higher mortality rates and worse functional outcomes.
Post Acute Stroke Facts
- Readmission Rates (Vahidy et al., 2017; Leppert et al., 2020)
- 12-17% readmitted within the first 30 days
- Up to 50% readmitted within 1 year
- Lack of Services (Bushnell et al., 2018; Olaiya et al., 2017)
- 45% of all individuals receive no post-acute services
- 87% of stroke survivors report unmet needs
- Return to Work (Duong et al., 2019)
- ~56% of people at 1 year
- ~66% of people at 2 years
Up to 17% of stroke survivors are readmitted within the first 30 days and up to 50% in one year. Reasons for readmissions include falls, fractures, recurrent strokes, and even other medical complications.
Forty-five percent of stroke patients receive no post-acute services at all, and 87% of stroke survivors report unmet needs in areas such as functional mobility and ADLs, access to services, and education regarding the prevention of future strokes. About half of stroke survivors return to work at the one-year mark, and by the two-year point, only 2/3 of stroke survivors have returned to work. These numbers are low.
Independence
- Facilitators
- Continued therapy post-stroke improves functional well-being
- Barriers
- Lack of services
- Sense of abandonment
- Grief with diagnosis
- Denial to rehab programs
Facilitators to independence after a stroke include ongoing therapy to improve their function and return to the community, access to financial assistance, mental health services, and support groups. Barriers are a lack of services and a general sense of abandonment as their friends move on with their lives and they have not been able to return to work or their hobbies.
Grief, along with a stroke diagnosis, is a big one. A stroke can cause a huge change in lifestyle and independence for people and their caregivers. Mental health services and support groups are lacking for stroke survivors. Denial to rehab programs is yet another barrier that limits their independence because they can not get in and work with the therapies to become independent.
With high readmission rates, especially in the post-stroke population, there is a large effort to bridge the gap between hospital and home.
Comprehensive Post-Acute Stroke Services (COMPASS)
- How it Works
- Educational materials at discharge
- Two-day follow-up phone call
- Clinic visit within 2 weeks
- Follow-up calls at 30 and 60 days
- Monthly quality metrics at each site
- Outcome assessments via telephone at 90 days
Current studies are going on throughout the country and globally discussing different models to achieve the goal of increased independence. One of the main models, still in development, is called the Comprehensive Post-Acute Stroke Services model or COMPASS. It is a clinician-led quality improvement model aimed at providing a supported discharge and transitional care for individuals discharged from the hospital.
At discharge, the post-acute care team gives patients educational materials. It follows up with them via a phone call two days after discharge to coordinate getting these patients in for a clinic visit within the first two weeks post-discharge. During these clinic visits, they meet with a medical team and a case manager to ensure that they are still stable from a medical standpoint, have all of their medications and therapies needed, and have follow-up appointments scheduled. There is also a phone call at the 30 and 60-day point to discuss ongoing needs.
The COMPASS model has been shown to decrease readmission rates and improve quality of life post-discharge, which makes sense because the patients are getting help after they leave the hospital.
Pros and Cons
- Pros
- Addresses multiple domains
- Customized to meet specific complex needs
- Easily adapted to meet specific needs
- Cons
- Short hospital stays
- Mild strokes or TIA can be missed
- Hospital workflow and staffing structure
- Insurance barriers
The pros of the COMPASS are that this model addresses multiple domains, from caregiver support, self-reported outcome measures, to interventions for self-management. It is customized to meet the specific and complex needs of stroke survivors. It is also easily adapted to meet the needs of other complex chronic conditions.
Identifying eligible individuals with stroke or TIAs is challenging, and hospital stays are short. For most TIAs, if they even make it to the emergency room, they are typically there for less than 24 hours. Incorporating this model into the hospital's unique clinical workflow and staffing structure is also challenging. It is also expensive as it requires several people dedicated to these post-acute services, depending on the hospital's size. There can also be insurance barriers.
Case Study Reintroduction J. K.
- J.K. is a 67-year-old female presenting after an unwitnessed fall with acute right MCA stroke, left shoulder hematoma, left 4th rib fracture, and left pneumothorax.
For those who did not attend Part 1, we discussed J.K.'s case in great detail. She is a 67-year-old female presenting after an unwitnessed fall with an acute right MCA ischemic stroke, left shoulder hematoma, and left fourth rib fracture. She also had a left pneumothorax. We followed J.K. throughout her acute care and inpatient rehab stay during the first course. Today, we are going to follow her into the home setting.
Home Health Rehabilitation-Home Health Care Team
- Patient
- Caregiver
- Therapists
- Case Manager
- Medical Team
This is a general overview of the home healthcare team.
Home Health Rehabilitation-Ongoing Medical Management
- Blood Pressure
- Mental Health
- Wound Care
- Stroke Prevention
Medical management remains important for stroke survivors to monitor and manage their blood pressure and medications to prevent additional strokes, provide mental health screening, and give wound care if needed.
For stroke prevention, medical professionals can work with patients to educate them on habits like smoking, obesity, and a sedentary lifestyle. They can also help them manage risk factors like renal dysfunction, hyperglycemia, and high blood pressure.
Home Health Rehabilitation-Benefits
- Cost Effective
- Effective at Improving ADL and Gait Performance
- Associated with Decreased 90-day Readmission Rate
Some of the benefits to rehab in a home health setting are that it is cost-effective and the patients make gains. I want to point out that home health rehab is not superior to inpatient rehab settings due to the intensive therapy that the patient receives in rehab. Still, the patients make gains when they are at home, so it is advantageous for some patients.
In fact, home health services are associated with a decreased 90-day readmission rate when discharged from the hospital and their inpatient rehab stay.
Home Health Rehabilitation-Home Health Evaluation
- Medical Chart Review
- Patient Interview
- Objective Assessments
- Plan of Care
- Goals
- Equipment/Orthotic Recommendations
- Discharge Planning
A home health evaluation for PT and OT will look the same throughout all sessions, including a chart review, patient interview, objective assessments, goals and plan of care recommendations, equipment assessment, and discharge planning.
Home Health Rehabilitation-Outcome Measures
OT Outcome Measures
- 9 Hole Peg Test
- Action Reach Arm Test
- Arm Motor Ability Test
- Assessment of Life Habits
- Box and Blocks Test
- Clock Drawing Test
- Canadian Occupational Performance Measure
- Capabilities of Upper Extremity Test
- Fugl-Meyer Assessment of Motor Performance*
- Montreal Cognitive Assessment
- Motricity Index
- Short Blessed Test
- Short Form-36
- Star Cancellation Test
- Stroke Adapted Sickness Impact Scale-30
- Stroke Impact Scale*
- Stroke Rehabilitation Assessment of Movement*
https://www.neuropt.org/practice-resources/neurology-section-outcome-measures-recommendations/stroke
PT Outcome Measures
- 5 Times Sit-to-Stand*
- 6-Minute Walk Test*
- 10–Meter Walk Test*
- Activities-Specific Balance Confidence Scale*
- Balance Evaluation Systems Test
- Berg Balance Scale*
- Chedoke-McMaster Stroke Assessment
- Fugl-Meyer Assessment of Motor Performance*
- Functional Gait Assessment*
- Motricity Index
- Postural Assessment Scale for Stroke Patients*
- Stroke Impact Scale*
- Stroke Rehabilitation Assessment of Movement*
- Trunk Impact Scale
https://www.neuropt.org/practice-resources/neurology-section-outcome-measures-recommendations/stroke
We are not going to review these outcome measures. These lists are for your reference. This is not an exhaustive list, and the measures with asterisks are highly recommended based on StrokEdge.
StrokEdge is a stroke evidence database to guide effectiveness and has a template for measuring the effectiveness and equality of outcome measures. It reviews many outcome measures for the stroke population and ranks them from highly recommended to not recommended for various practice settings depending on patient chronicity.
The outcome measures on the slides are the ones that are highly recommended. If you want to see all of the other outcome measures, you can visit the website, which is linked for you at the bottom of each slide. These are the outcome measures specific to the home health setting.
There is another set of slides in the outpatient section that we will cover.
Home Health Rehabilitation-Interventions
- Strengthening
- Balance
- Vision/Cognition
- ADLs/IADLs
- Mobility
- Durable Medical Equipment (DME)
- Education
- Home Modifications
- Community Resources
These are some general interventions to use with stroke patients in the home health setting. Again, this is not an exhaustive list, but these are the ones that we are highlighting today. We will talk about all of these in detail in the following slides.
In the home health setting, most patients receive about three hours of therapy or less last per week, depending on the type and frequency of services. This is compared to 15-plus hours a week at the acute rehab level.
Looking at where they are in their critical window of recovery, home health therapists are likely catching these patients during the three to the six-month timeframe where they are able to make the most gains post-stroke. With less frequent therapy, though, we must get creative and come up with ways to weave traditional therapy into their daily activities and routines so that they continue to make progress despite the less frequent therapy.
Strengthening
- Exercises
- Mirror Therapy
- Video Games/Apps
- Household Activities
- Functional Mobility
- Get Creative!
With traditional strengthening exercises, we want the recommended number of sets and reps to be challenging enough for the patient to make gains. We also want to consider exercises that require the coordination of multiple muscle groups, like bridges, instead of isolating individual muscles or a reaching task in place of simple shoulder flexion.
The use of mirror therapy is cheap and easy to implement at home.
Apps and video games are much more readily available these days. The use of multimodal mental practice is another inexpensive and fairly simple intervention to perform in the home setting. Using this intervention, the patient observes a task, follows that with mental practice or imagining themselves performing a task, and then completes mass practice to increase their upper extremity strength or whatever they are working on.
The use of household activities and functional mobility to build strength is when patients are most likely to follow through, especially when they are not in therapy. These include things like putting dishes or laundry away. These are great activities to work on strength, balance, and coordination to accomplish PT and OT goals.
You can get creative and tap into their hobbies. What do they like to do? Doing a puzzle may not be a specific therapeutic intervention. However, you can have them complete the puzzle in standing, using their hemiparetic arm for standing balance, endurance, upper extremity strengthening, and coordination. Dancing is another great activity where you can target many different impairments, and it is applicable to patients who are low to high level.
Strengthening tasks, in general, are interdisciplinary and work on overall strength to address both PT and OT goals. The next slide shows a strengthening video. Alaena is going to jump in and talk about it.
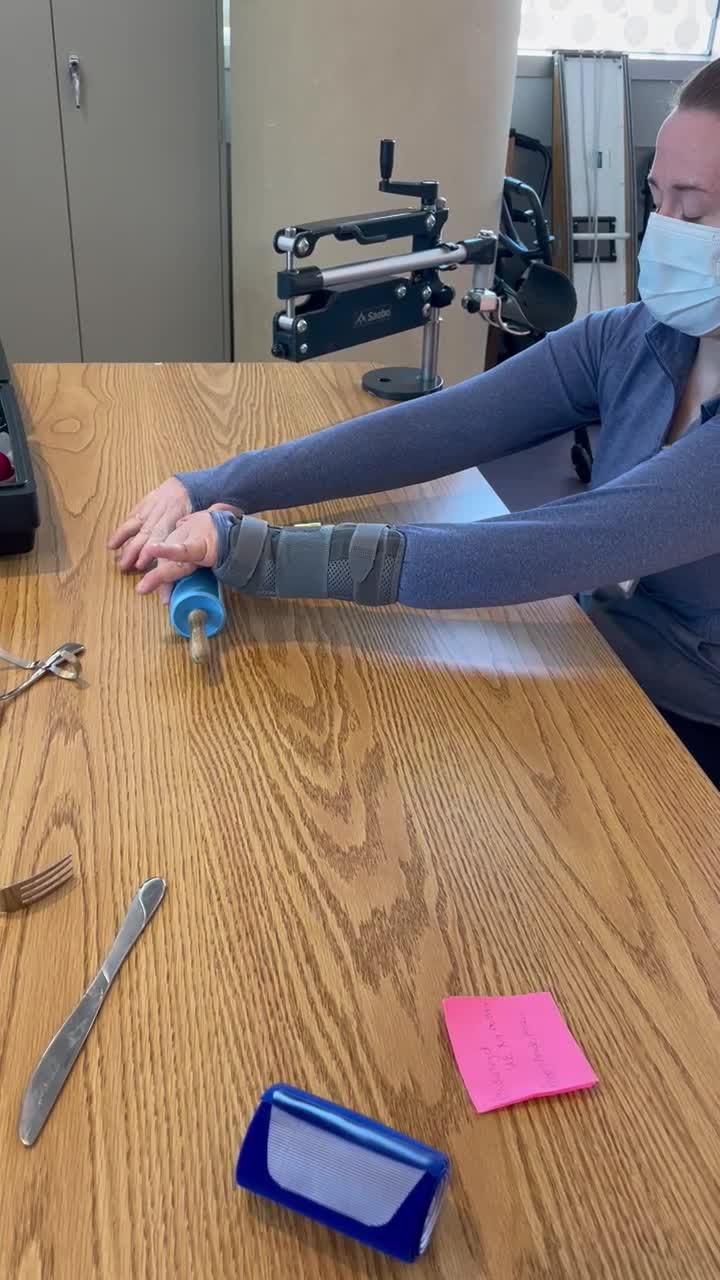
Alaena: Before I play this video, I want to explain it. It is an example of an optional treatment intervention for strengthening in the home setting. I want you to keep in mind that to have a creative and motivating session, it does not have to be complex, as Katie said. You can use items that are easily accessible within the home, which will also help keep the patient engaged.
In this video, you will see the patient using a mirror from a portable mirror box from our clinic, but you can use any available mirror. This activity gives the patient the opportunity to reach shoulder height. She has a splint on the unaffected arm, which was like a modified CIMT intervention. We are now going to play the video so you can see how the patient is moving.
Video 1
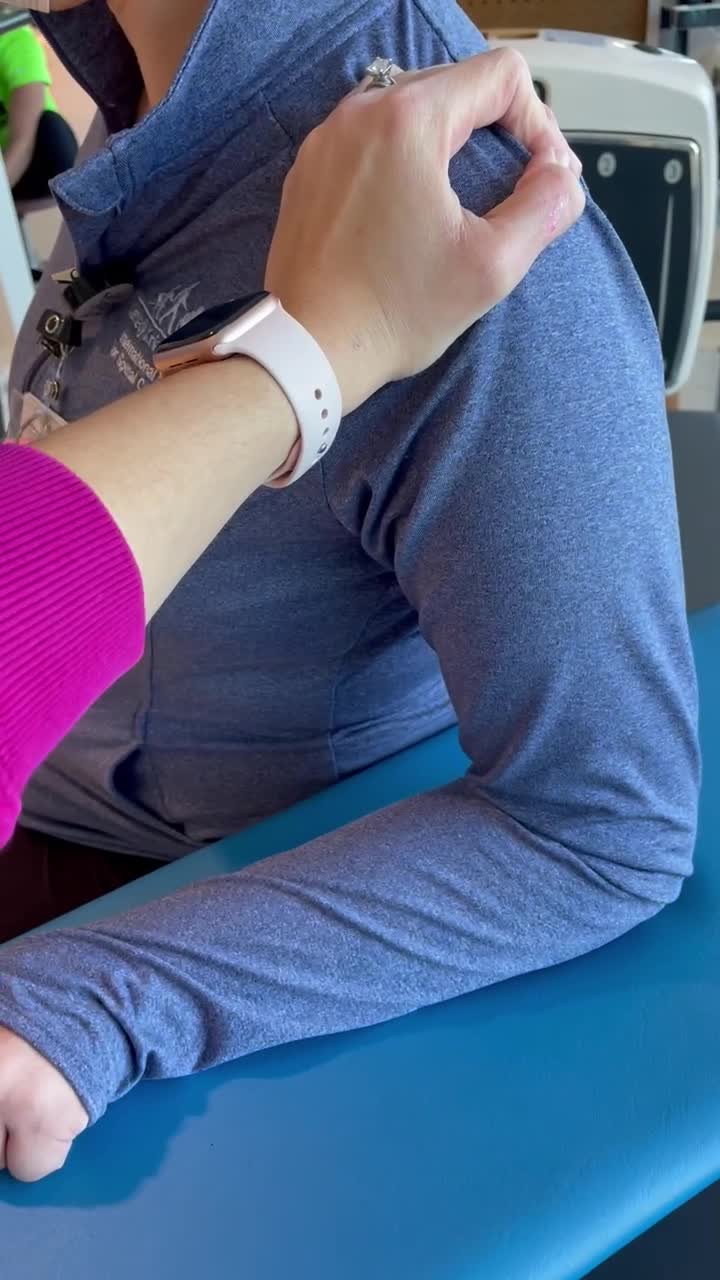
This treatment intervention aims to increase accuracy, coordination, and strength to meet ADL tasks like dressing, meal prepping, and grocery shopping. Be mindful that when you are in the home setting and doing any activity with a hemiparetic or weaker arm, they may tire after four to five reps. You may want to use more of a preparatory activity and then go into the actual ADL task. You can build endurance by increasing reps, the height of items, or adding some weights if appropriate.
Balance
- Strength and Coordination
- Gaze Stabilization
- Perturbations
- Dual/Multi-Tasking
- Safety
- Fear of Falling
- Make it Fun!
Katie: Balance is the integration of somatic sensory, vestibular, and visual systems, all of which can be impaired due to stroke. It is important to work on improving balance with all of these patients. Balance interventions can include strength and coordination by addressing the main core and lower extremity muscles, like the tibialis anterior and quads. We also want to address the coordination of movement to produce effective balance strategies like taking a step or preventing falls. Gaze stabilization exercises like VOR (Vestibular Ocular Reflex) and perturbation training will help improve the reaction time and effectiveness of their balance so they may have enough strength in their arm to reach out to the side or catch themselves when working in a seated position. They need to do it fast enough to prevent a loss of balance.
Dual and multitasking ensure they can keep their balance while concentrating. Performing a seated or standing ADL is multitasking and can be difficult for patients with significant balance deficits. They are concentrating so hard to maintain their balance, and now we are adding additional tasks. We want to give them balance activities as part of their home exercise program that they can safely practice in their home.
A fear of falling can cause people to do unsafe things, like reach for a piece of furniture or wall four feet away or furniture on wheels. It is important to address their fear of falling and educate them on safe ways to move within their home.
Lastly, you can use virtual reality if you have access to those devices. They can also work on balance while doing a hobby they like. Balance tasks are interdisciplinary, and working on balance will address PT and OT goals in almost every patient.
Now, we are going to discuss vision and cognition as it relates to treatments in the home health setting.
Vision and Cognition
- Restorative
- Mental practice
- Repetitive task practice
- Compensatory
- Strategies
Alaena: Visual and cognitive impairments will affect participation in ADLs, IADLs, and mobility. We can break this up into restorative versus compensatory strategies to help the patient be independent in those activities.
Restorative interventions include using things like mental practice, which can be as simple as imagining the task components and completing them prior to the activity, followed by repetitive and mass practice of that activity. We want to set the patient up for success by giving the patient making it routine or using the same environment. We can then add new things to that activity to increase their independence.
This can be as simple as getting dressed using an overhead shirt over and over. We want them to start to attend to their arm if that is our goal. We can then have them try a different type of shirt that is smaller or has buttons to get them even more independent. From a PT point of view, we can add more obstacles as they ambulate throughout the house.
Our goal is to keep that patient as safe as possible in their home environment. This might mean adding compensatory strategies throughout the house. We can use a combination approach or a restorative approach only. However, when we are not there, we need to educate the client and family members on how compensatory strategies will help increase their independence and allow them to monitor how vision and cognitive deficits are progressing. We can take some of that stuff away if they are getting better.
Compensatory strategies can include looking at a daily logbook with reminders, post-it notes, phone auditory reminders, or errand lists. Visual strategies like scanning, red tape in the room to highlight things, light sensors around the room, and motion detectors if the patient is unsafe in the middle of the night. If the patient is impulsive or has short-term or long-term memory loss, alarms on the bed or doors can reduce the risk of falls. Overall, we want to encourage appropriate visual aids and adaptive equipment, especially if there is double vision or processing issues.
We also want them to follow up with a neuro-ophthalmologist. We can facilitate this by sending a note to the primary care physician or talking with the client and family to follow up on their own.
ADLs/IADLs
- Restorative
- Compensatory
- Adaptive equipment
- Orthotic
- DME
The next area involves ADLs and IADLs. Again, there are both restorative and compensatory approaches. From a restorative standpoint, we will use task analysis to figure out how to break down the ADL task for specific movement patterns and how we can help them increase their independence. Exercises could focus on all of those deficit areas, and we can also educate them in proper kinematics and use biofeedback and functional e-stim if appropriate.
Compensatory strategies include adaptive equipment to increase independence, such as buildup utensils, curved bowls, Dycem, magnets for clothing, and elastic shoelaces. This equipment can be reevaluated as the patient progresses.
We want things that we can quickly adapt, like Coban wrap. For example, if you notice someone with poor grip strength for feeding tasks, Coban can be used to build up utensils. You can also look at orthotics, such as u-cuffs, t-bars, and any other durable medical equipment or DME. Items include reachers, sock aid, ambulatory devices, and commode chairs. Grab bars, if needed, are pretty reasonably priced from local stores.
You can use this small bag of tricks at any time. You do not have to recommend that the client buy all new things. You can evaluate and monitor the effectiveness of each of those devices as the patient progresses in their diagnosis.
Mobility
- Goal-Driven
- DME Evaluation/Education
- Obstacle Negotiation
- Progression
Katie: Now, we will talk about mobility. In the home health setting, we will talk about goal-driven mobility interventions. The best way to talk about this is with some examples. Our first example is a patient that is home with a first-floor set up with a hospital bed in the living room, and they want to get back to their own bed upstairs for some privacy. We can work on bed mobility in their hospital bed with the bed flat. This activity can also be given as a home exercise program so they can work on this when therapy is not there. We also want to look at stair negotiation so they can get up into their own bed.
Another example is a patient that has been stuck sitting on only her bed or kitchen chair because all of the other surfaces in her home are too low. We can work on sit-to-stands from various height surfaces to help the client get back to being able to sit on something comfortable, which is a huge quality-of-life issue in some patients. We want to practice all of the different surfaces within the home, including a tub bench or a bedside commode. We can change the heights so that they can practice going to surfaces that are slightly lower but still have an armrest so that they can get up.
We can introduce assisted devices, equipment, and bracing as needed.
For obstacle negotiation, there are two points to be made. First, we need to eliminate obstacles. Can you rearrange their setup, pick up throw rugs, move furniture, and clean up the floor? Secondly, we want to ensure they can safely negotiate their environment's static and dynamic obstacles. Can they get around their coffee table that has legs angled out? Is their balance good enough to negotiate dogs and cats (dynamic obstacles) moving around?
For progression, patients being seen in rehab in the home setting are considered homebound. We need to think about how to progress these patients toward community reintegration, which is ultimately going to be their goal.
DME Recommendations
- Evaluation
- Education
- Modifications
- Recommendations
Durable medical equipment (DME) is another area where PTs and OTs frequently collaborate. Depending on where the patient was discharged from and their discharge circumstances, they may have come home with no DME or even the incorrect one. Doctors discharge patients all the time without rehab evals. Or, perhaps therapy wrote in their notes that the client needed a tub bench or a bedside commode, but the insurance company did not cover it, so they came home without one. The client may not be able to get the equipment or know where to start.
You also want to ensure the family and client know how to safely use the equipment. Is their equipment adjusted to the proper height? Do they know how to do skin checks? We may need to modify the equipment, like using additional padding for patients who are prone to skin breakdown or building up a handle.
You can also help them assess the need for other equipment, give them resources, and help them to obtain them.
Education/Home Modification
- UE Positioning
- Injury prevention
- Orthotics
- Follow up
- Safety
- Fall prevention
- Stroke prevention
- Emergencies
PT and OT collaboration during patient and family education is essential. We want to deliver the same message and recommendations to keep our patients safe.
For upper extremity positioning, we need to ensure that the patient and their caregiver are paying attention to the hemiplegic extremity at rest and during movement to prevent injuries, as sensation and sometimes attention to the extremity can be impaired. For example, we do not want it to get stuck underneath their body when they are in the bed or exposed to extreme heat around the stove or when washing their hands.
We want to approximate the shoulder joint to prevent subluxation or worsening subluxation. We can evaluate for orthotics or determine if the use of a sling for their hemiplegic upper extremity is appropriate during mobility.
We also want to educate on fall prevention strategies, such as the use of a reacher when things fall on the floor, putting everything within their reach, placing assisted devices close by so they do not have to move without it or reach way out for it, making sure that they have proper lighting, and removing trip hazards.
For stroke prevention, we want to review the signs and symptoms of a stroke, educate when to call for help, and take the patient's vitals every session. It is also important to reinforce the use of medications prescribed by the doctor, especially for patients who tend to be non-compliant. You can discuss how to safely exit the home in case of an emergency with their new mobility device.
And how do you call for help in case of an emergency?
- Home Evaluation
- Home Modifications
- Home Rehabilitation Program
During the home evaluation, we need to assess their first-floor setup, bathroom, and sleeping arrangements. Are they able to access the entry and exit to the home? We also want to remove obstacles from the house, like throw rugs and cords, and rearrange furniture if needed. Additionally, we can move chairs to places where they might need a rest break and use colored tape for patients with visual issues.
We can implement checklists to help the family and patient implement these things. Visual schedules and step-by-step instructions can also be helpful.
There is generally a low adherence to home exercise programs throughout all settings. Keeping them motivated by focusing on household activities, functional mobility, and hobbies may increase adherence.
Community Resources
- Mental Health Support
- Community Reintegration
- Free Resources
For community resources, we can give our patients and their families resources for stroke support groups, caregiver support groups, and DME loan closets. There may also be local community reintegration programs, which we will discuss later in this presentation.
Other Considerations
- Cognition
- Caregiver Support
- Telehealth Visits
Cognitive impairment and memory deficits are negatively associated with improvements in function. It is important to screen these patients and refer them to speech therapy or other medical professionals as needed.
Make a point to check in with a caregiver to see how they are doing and if there are any other resources they need. Caregiver burden is real, and we want to ensure that we provide these people with the resources to prevent burnout as much as possible. Does the patient qualify for a home health aide to take the stress off of the caregiver? We can connect them with a case manager to see what else they need in terms of support.
Regular follow-up for these stroke patients is key. If somebody is sick or they are on vacation, consider a telehealth visit. The effectiveness of telehealth visits has been similar to traditional treatments with stroke patients, so it is a feasible way to keep up with regular sessions.
Home Health: Interdisciplinary Approach
- Screening for Other Disciplines
- Communication
- Education
- Supporting Other Disciplines
Ways to implement an interdisciplinary approach in the home health setting include screening for other disciplines, communicating with other team members to see the patient to create a more comprehensive care plan, and communicating safety concerns, barriers to progress, and general treatment plan so that the other treating therapists can reinforce the techniques you are using.
Communication does not have to be a huge chunk of time out of your day. We all understand we are all short on time, so send a quick email or make a phone call between patients while you are in the car. You can also leave paperwork with the patient to show their other therapists so that the interdisciplinary communication does not feel like so much of a burden.
Collaboration with the patient and family is another way to implement an interdisciplinary approach in the home health setting. We want to educate them on stroke prevention, safety, and fall prevention.
Last but not least, we must support the other disciplines to maximize patient outcomes. Is there anything that you can add to your session that would make a difference? Can you modify your session to work on other disciplines' goals, like having the client sit up on the left side of the bed instead of the right? Can you prioritize exercises in a seating position instead of bed level so that they can work on their sitting balance? Small changes can make a big difference.
Home Health: Case Study J. K.
- Acute Rehab LOS: 20 days
- Discharged home with home health PT f/u
- The caregiver will be home full time x2 weeks
- Works 5 days/week from 9-5
- Seen for home health PT/OT evaluations ~ 4 days post-discharge
Now we come back to our case study for J.K. This is a 67-year-old female, status post a right MCA infarct. She was in acute rehab for 20 days and discharged home for home health follow-up. Her caregiver is home with her for two weeks and then has to return to work. She was seen for home health PT/OT evaluations about four days post-discharge.
- Functional Status
- Bed mobility and transfers with supervision
- Ambulating 75 ft and stair negotiation with SPC and CG A
- Basic ADLs bed level/seated with supervision
- Toileting with CG A
- Concerns for safety given ongoing L inattention
- Patient Goals
- Improve independence in toileting and ambulation so her caregiver can return to work
Her bed mobility and transfers are completed with supervision. She is ambulating 75 feet and doing stair negotiation with her cane with contact guard assistance. Her basic ADLs are at bed level or seated with supervision, and toileting is with contact guard assistance. There are ongoing concerns for safety, given her left inattention.
We have a problem. The patient is not independent with any mobility or ADLs at this time, and she will be left alone for eight hours a day once his caregiver returns to work in two weeks.
- Discussion Points
- Prioritizing needs
- Plan of care
- Time frame
We must prioritize needs to see what to address. We should address safety first by completing a home evaluation, making any recommendations for modifications, and providing education about emergencies, the signs and symptoms of stroke, and what to do if there is a fall. We can start to create a plan for maintaining the patient's safety during that eight-hour window when she is alone and assist her with any resources for DME that she may need to make that happen.
The plan of care includes three times a week sessions initially for each discipline, if possible. We then collaborate to get a firm plan for how to progress this patient. For example, if the PT and the OT teach the same transfers and provide the same recommendations for her safety, what will this plan look like?
The patient currently needs assistance when she is walking due to her left inattention. Since she is not going to have assistance during these eight hours, we may need to consider a wheelchair for mobility when she is alone. She does not have a first-floor setup because of her bathroom situation. We must set her up on the second floor so that she does not need to go up and down the stairs, including the caregiver providing food and other items before they leave.
For DME, besides the wheelchair, the client may need a bedside commode and a gate for the top of the stairs, depending on her setup. With the left inattention, if she is going to be wheeling herself past a flight of stairs, we need to ensure there is a gate.
We can also put up visual reminders for left attention. Setting up a place to keep her phone in an emergency is crucial. Doing one or two practice runs may be important before the caregiver returns to work.
The OT can work on toileting, toilet transfers, basic meal prep, opening containers, self-feeding, and everything that she's going to need to be independent during that time by herself. They can also work on cognition and safety, like creating a list of emergency numbers and a fall alert system. Visual reminders, like checklists or step-by-step lists, can be helpful for daily tasks. Alarms on the phone can also support this.
PT interventions can include bed mobility, transfer training, and wheelchair mobility. As we think about transfers, we need to consider equipment setup. This patient's biggest issue is her left inattention and transfers toward the left will require more safety assistance. If we cannot improve these transfers toward the left to an independent level before the caregiver returns to work, can she transfer only toward the right? The answer is yes, but to do this, you have to create a triangle with her bed, commode, and wheelchair at the bedside so that she can go from the edge of the bed to the commode to the wheelchair and back to the bed, all toward the right. It is not an ideal setup, but it is possible. We may need to move furniture and barriers and practice turning while negotiating obstacles and doorways. We may need to provide education on brakes so that she remembers to lock both sides.
I would like to comment quickly on stairs. In general, we are going to have this patient avoid stairs when she is alone, but we should consider teaching her how to bump down on her bottom in case of an emergency when she is alone. After we have achieved the primary goal of progressing her to independence during those eight hours that she has to be left alone, we can shift our focus to additional tasks to help progress her overall function.
- Initial Interventions
- ADLs
- Cognition/Safety
- Bed mobility
- Transfers
- WC mobility
- Progression
- Grade activities
- Focus more on IADLs and community reintegration
- Home exercise program
OTs can help her work on independence with her ADLs, which will help to take the burden off of her caregiver and meal prep, like using a microwave or stove. We can then start to work on community reintegration, like grocery shopping.
PTs can work on gait training, improving her overall distance and endurance, balance training, obstacle courses, perturbation, and reactive balance training to help prevent falls if she bumps into an obstacle or a wall on her left side, given her inattention. Doing reaching and weight shifting for balance will help with OT goals. PTs also work on transfer and stair training.
OT/PT Goals
- Examples of Possible OT Goals:
- Patient will perform toileting activity independently with use of grab bars
- Patient will be able to perform standing reaching task for 5 minutes in prep for IADL meal prep activity
- Patient will be able to attend to left side while performing ADL tasks without verbal cues for 75% of task
- Patient will increase left UE strength by reaching for object at shoulder height in 3 out of 5 trials in prep for independence needed for community reintegration
- How Can PT Help Facilitate These OT Goals?
- Reaching exercises during balance training focusing on L UE reaching
- Transfers between various surface heights
- Incorporating L UE weight bearing during exercises
- Increasing awareness to the L side during all functional tasks
These are some examples of possible OT goals, and they include performing toileting using grab bars, performing reaching tasks in standing in prep for IADL activities, attending to the left side without verbal cues, and increasing upper extremity strength.
The PT can help facilitate these OT goals by having a patient reach with their left upper extremity when performing dynamic balance-reaching activities or working on transfers between surfaces of varying heights. PT can incorporate left upper extremity weight-bearing throughout their sessions as well and continue to work on the awareness of the left side during all functional tasks.
These are all examples; each discipline should plan its sessions with its own goals. Helping a patient to meet their goals in a different discipline should not be the purpose of your session. What we are talking about here is being mindful of the patient's goals with the other discipline and building in opportunities or small changes in your session that are not disruptive.
- Examples of Possible PT Goals:
- Patient will perform bed mobility independently without cues
- Patient will perform SPT to/from surfaces of varying heights independently with SPC
- Patient will negotiate obstacles and furniture within home while ambulating with SPC independently and no cues for left attention
- Patient will propel manual wheelchair with R UE/LE independently
- How Can OT Help Facilitate These PT Goals?
- Incorporate exercises in supine and sitting to encourage bed mobility
- Uneven transfers during toileting and other ADLs
- Reinforce wheelchair training and safety
- Incorporate balance training during standing ADLs
Some examples of PT goals for this patient in the home health setting include bed mobility, transfers, negotiating obstacles while ambulating, and propelling her wheelchair independently. OT can help facilitate these goals by focusing on bed mobility techniques when transitioning in and out of supine for exercises or working on transfers to a low toilet. This will reinforce wheelchair training and safety. Lastly, the OT can incorporate balance training into their session while doing standing ADLs.
Outpatient Rehabilitation: Overview
- Clinic Setting
- Underutilized
- Single vs. Multiple Disciplines
- More Chronic Cases
- Focus on Specific Goals
Here is an overview of outpatient rehabilitation, which is traditionally provided in a clinical setting. It can be an underutilized service post-stroke due to the many barriers that this population may face, including transportation, insurance, and caregiver support barriers. There also may be limited clinic options that focus on the neurological population. It is important to note that post-COVID, some of these services are even more underutilized because of the lack of caregiver support and staff and transportation shortages.
The outpatient clinic may have a medical team on the site as well as a social worker and other support staff. There are also PT-only or OT-only clinics.
We tend to see more chronic cases in the outpatient setting, but it is not unheard of to see people in the subacute stage. Once they are in the outpatient setting, we tend to see more specific patient goals. This could be as simple as the patient wanting to be able to open a specific door to get into their closet.
Outpatient Rehabilitation: Medical Management
- Blood Pressure Management
- Mental Health
- Stroke Prevention
- Dependent on Clinic Policies
Medical management is different in the outpatient setting, and it can also differ at every clinic. Each clinic has protocols and procedures. For example, blood pressure could be checked at every session, or it could just be checked with some new interventions. There should be protocols about what to look for, document, and when to alert the medical staff should be alerted. The particular steps, like sending the patient to the ER or urgent care, need to be noted. Typically, the patient will not be able to come back to therapy then until cleared by a doctor.
In outpatient, we are still focusing on the mental health component, knowing that this population and caregivers are at an increased risk for depression, as Katie touched on in home health. If there is no social worker on site, gathering resources or reaching out to their primary medical professionals may be helpful for the patient or family to work through their mental health issues.
We also want to educate them about stroke prevention, which might include encouraging the patient to attend follow-up appointments with their doctors, taking their blood pressure if appropriate, and providing them with a home rehab program to keep them active when they are not in therapy.
Outpatient Evaluation
- Medical Chart Review
- Patient Interview
- Objective Assessments
- Plan of Care
- Goals
- Equipment/Orthotic Recommendations
- Discharge Planning
The outpatient eval is similar to the other settings we have talked about in parts one and two of this series. It includes a medical chart review, a subjective patient interview, objective measures, a plan of care, goals, equipment and orthotic recommendations, and discharge planning.
OT Outcome Measures
- 9 Hole Peg Test
- Action Research Arm Test
- Arm Motor Ability Test
- Assessment of Life Habits
- Box and Blocks Test
- Canadian Occupational Performance Measure
- Dynamometry
- Fugl-Meyer Assessment of Motor Performance*
- Graded Redefined Assessment of Strength, Sensation, and Prehension
- Mini Mental State Examination
- Modified Ashworth Scale
- Motor Activity Log
- Motricity Index
- Pinch Test
- Short Form-36
- Stroke Adapted Sickness Impact Scale-30
- Stroke Impact Scale*
- Stroke Rehabilitation Assessment of Movement*
- Stroke Specific Quality of Life
- Jebson-Taylor Hand Function Test
- Wolf Motor Function Test
https://www.neuropt.org/practice-resources/neurology-section-outcome-measures-recommendations/stroke
Again, this is not an exhaustive list of the OT outcome measures. The ones that have asterisks at the end are recommended by StrokEdge, and there is a website at the very bottom if you want to look at a more exhaustive list.
PT Outcome Measures
- 5 Times Sit-to-Stand*
- 6-Minute Walk Test*
- 10–Meter Walk Test*
- Activities-Specific Balance Confidence Scale*
- Balance Evaluation Systems Test
- Berg Balance Scale*
- Chedoke-McMaster Stroke Assessment
- Fugl-Meyer Assessment of Motor Performance*
- Functional Gait Assessment*
- Motricity Index
- Postural Assessment Scale for Stroke Patients*
- Rivermead Motor Assessment
- Stroke Impact Scale*
- Stroke Rehabilitation Assessment of Movement*
- Trunk Impact Scale
https://www.neuropt.org/practice-resources/neurology-section-outcome-measures-recommendations/stroke
The ones with asterisks are recommended by StrokEdge.
Outpatient Rehabilitation: Interventions
- Robot-Assisted Therapy
- Constraint Induced Movement Therapy (CIMT)
- Mirror Therapy
- Task-Specific Training
- Neuromuscular Re-education
- Functional Electrical Stimulation
- Aquatic Therapy
- Gait Training
The following list of interventions is a combination of PT and OT interventions. We will talk about them in the next couple of slides, and we will tease out how each discipline uses them differently and complimentary when creating treatment goals.
Robot-Assisted Therapy
- Intervention Automation
- Need mass practice for beneficial patient outcomes
- Can provide a more consistent and efficient environment for mass practice
- Recorded data can be used to track progress and provide feedback to the patient
- Designed to augment and activate muscles in synergistic patterns and promote neural plasticity through repetitive motor tasks
First is robot-assisted therapy. It is based on mass practice and performed in a consistent and efficient environment. The feedback is designed to augment and activate muscles in synergistic patterns to promote neuroplasticity through repetitive motor tasks.
When you use a robot-assisted device, you will get more reps than in traditional therapy because the patient might be a little bit more motivated.
Up next, we have a video that shows an example of this in my clinic. The device is called the AMADEO, and it is used mainly for fine motor strengthening. There is a cuff that the patient's forearm goes into.
Additionally, in the video, you will see that each of the fingers has magnets on the ends and is connected to the device. The device goes through different modes. It starts with a preparatory mode, and you can do passive range of motion, active assist range of motion, and tone reduction, which is via the velocity of the movements. There is also a vibration that goes straight to the fingers. The idea is that after you prime the neuro system, you then move into different games. Let's take a look.
Video 2

The patient is moving their fingers in flexion and extension while trying to participate in this game. The graphics and the visual games are not great, but they keep the patient motivated. You can do different modes on this device as well.
You can also use force versus a range of motion. For example, if someone has maybe trace movements, the force allows them to still play in the game. The therapist can then change the threshold to 50% or 75% of the motion, which is awesome.
In OT, there is a plethora of robot-assisted options, both unilateral and bilateral.
- Robot-Assisted Outcomes
- OT (Hung et al., 2019)
- Unilateral and bilateral options
- Provides different benefits for people
- Unilateral: increase motor function and decrease tone
- Bilateral: potentially improve multiple power output
- PT (Calabro et al., 2021)
- Improvements in balance and lower limb motor function
- No significant differences in gait compared with conventional therapy
- Limb activation can improve midline perception in patients with unilateral neglect
- OT (Hung et al., 2019)
Each robotic device provides different benefits for the patient. Unilateral robotics have been shown to increase motor function and decrease tone, whereas bilateral ones can potentially improve multiple power output. Different robotics provide unique benefits, and this can also be patient-specific. It is not one size fits all. You can have two people with the same diagnosis and similar trajectories, and they respond differently to the devices. Examples of OT robotics include the Armeo, InMotion, the upper extremity exoskeleton, Bi-Manu-Track, Gloreha, and Meant to Move.
For PT, robotics show improvements in balance and lower limb motor function. There have not been any significant differences in gait compared to conventional therapy, but limb activation can improve midline perception in patients with unilateral neglect. Examples of PT robotics include overground exoskeletons, such as the ReWalk, Phoenix, and Indego, body weight support treadmill exoskeletons, and effective devices, such as the G-EO.
CIMT
- 3 Standard Components
- Restraint of the unaffected limb
- Intensive practice (massed practice)
- Reinforcement (shaping)
Next is constraint-induced movement therapy, or CIMT. CIMT is a neurological treatment designed to improve upper extremity motor function after a stroke. It improves the affected limb's ability by restraining the unaffected limb. This can be done using gloves, orthotics, slings, or, like in Figure 1, a simple fabrifoam.

Figure 1. Example of CIMT.
The therapist focuses on the intensive and mass practice of functional movement patterns to increase independence in functional goals and tasks. The patient gets feedback either verbally from the therapist, visually using a mirror, or even through auditory cues.
Due to the intensity of CIMT, a modified version may be ideal in this setting. In general, CIMT has been shown to be feasible and effective in the older and chronic stroke population.
- Pros
- More improvement was noted with right-sided lesions
- Promotes motor function recovery
- Enhances plasticity of dendrites and dendritic spines in the ipsilateral and contralateral sensorimotor cortex
- Cons
- Needs good caregiver support
- Hard to replicate the exact protocol
- Transferability between the clinic and real life
Some of the benefits of CIMT have shown improvements with right-sided lesions. It promotes motor function recovery and enhances the plasticity of the dendrites and the dendritic spines in the ipsilateral and contralateral sensory-motor cortex. The cons include the need for good caregiver support, especially with a patient that has cognitive deficits for the carryover in the home. It is hard to replicate the exact protocols in varying environments, and the exercises may not transfer to real life. It is important to note that the research has been more utilized in OT versus PT.
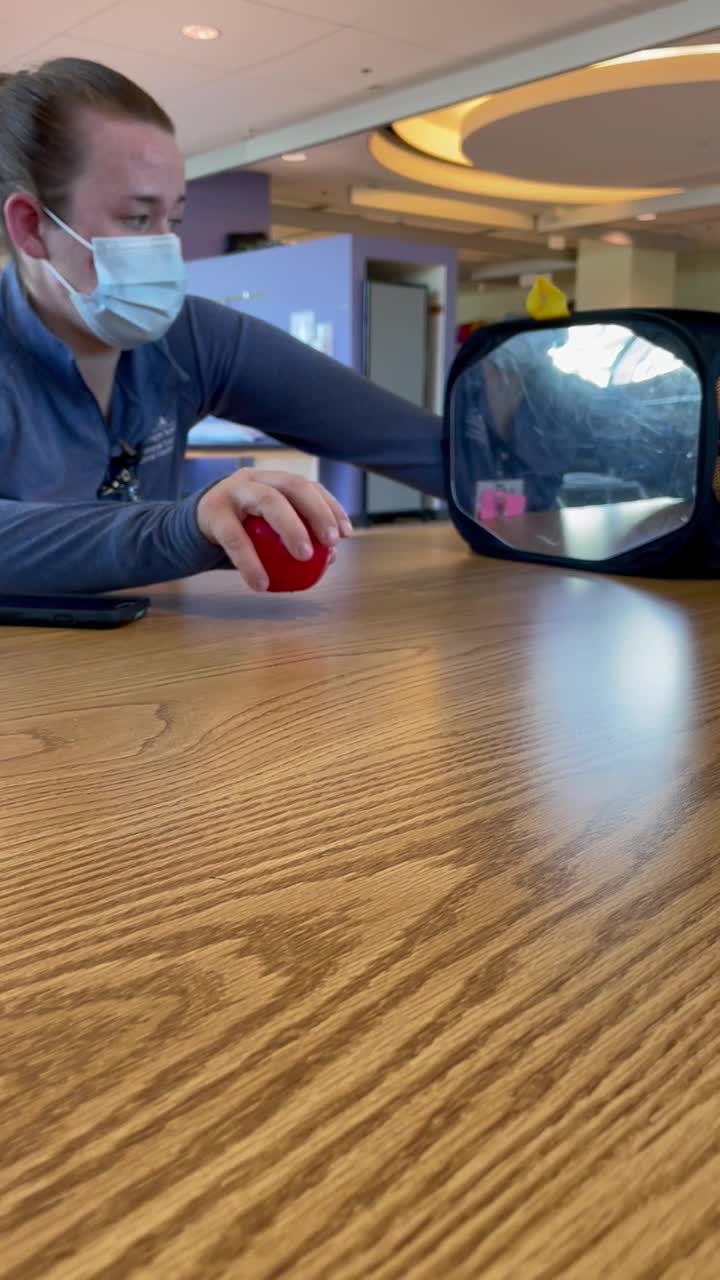
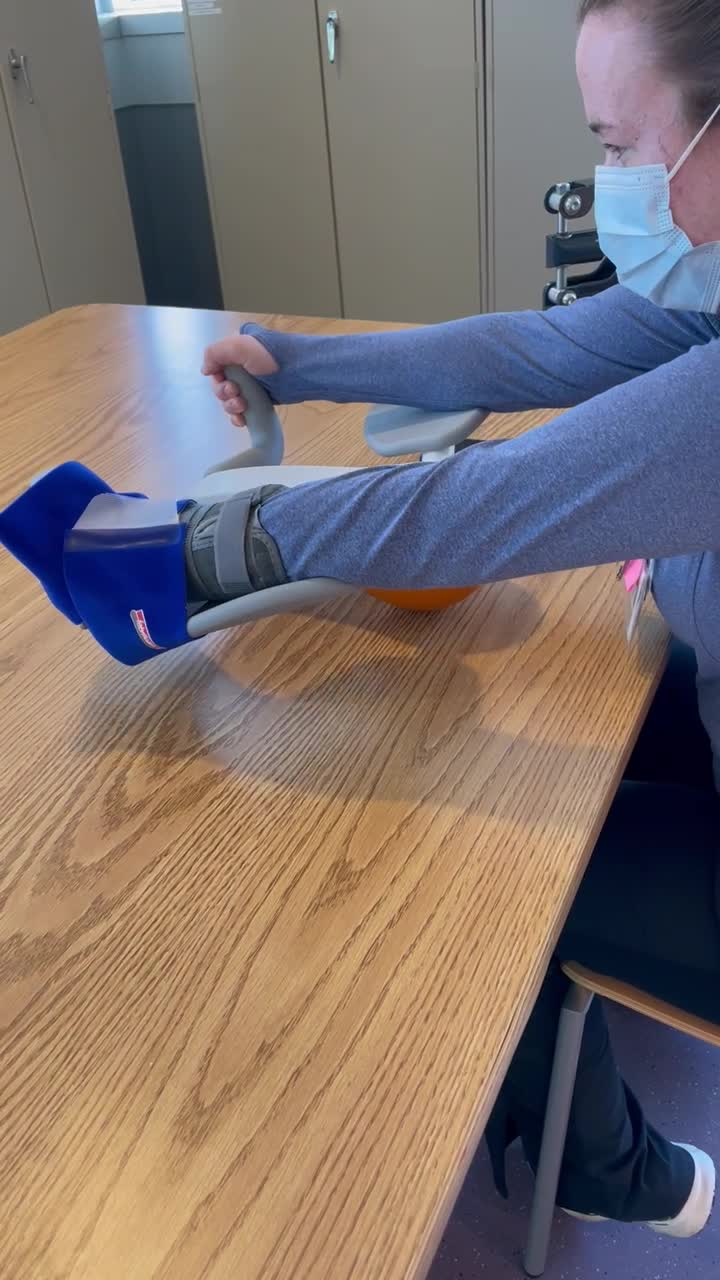
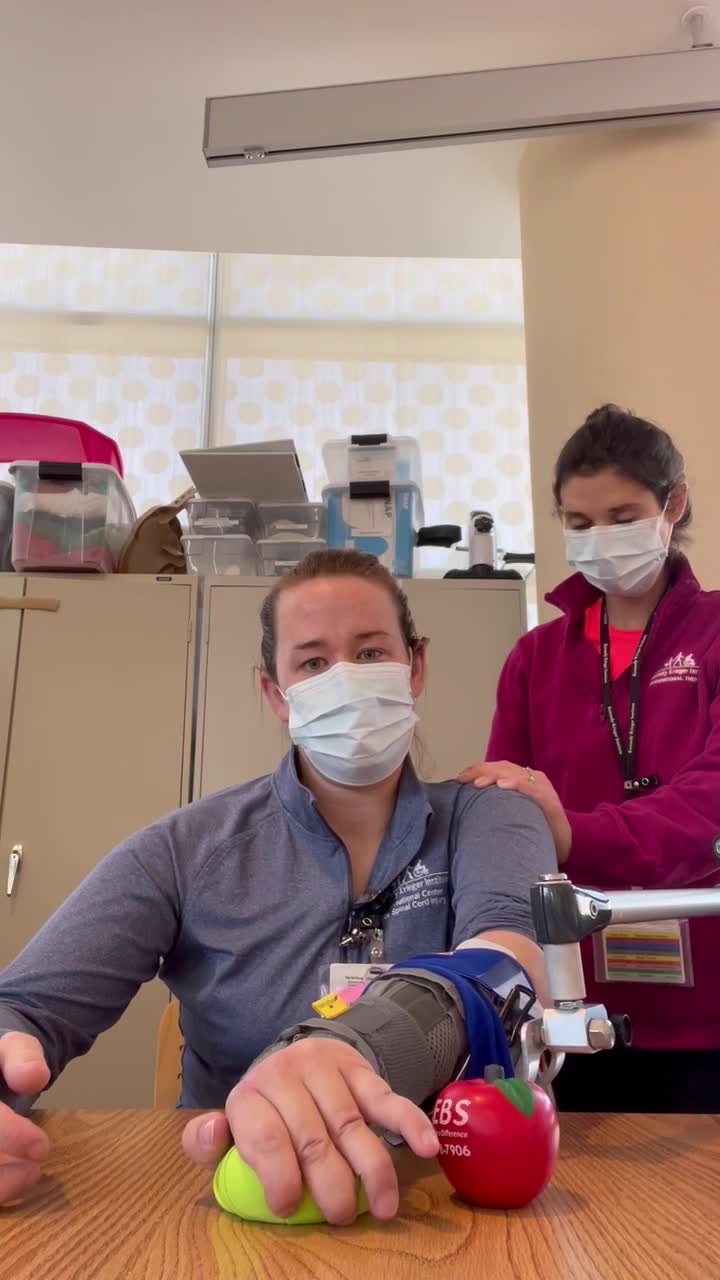
Here is another video showing CIMT.
Video 3

Constraint-induced movement therapy can also be done in standing to support PT goals. I know it is simple and can be boring, but it is motivating to patients. I can say, "I want you to tap the red ball two times," and then after that, "I want you to tap the ball two times, then go to the yellow ball." I can continue to add to this to work on three-step commands. It is a great way to work on that short-term memory, dual-tasking, and using different shoulder muscles within the shoulders. As she is reaching, you can also see trunk movement.
Mirror Therapy
The next intervention is mirror therapy. This allows for the use of a mirror to reflect some movements of the less involved upper extremity as if it were the more affected limb.
- Pros
- Inexpensive
- Easy to use
- Cons
- Inconsistent treatment dosing
- Recommended to be used as an adjunct
The parietal, frontal, and premotor brain regions become activated simply by observing the action when doing this intervention. It is a fairly inexpensive and easy-to-use treatment and can be paired with other interventions, such as e-stim. However, the research has shown that there are inconsistencies in the treatment dosage, and this needs to be used as an adjunct therapy.
In Figure 2, the unaffected arm is outside, and the affected arm is in the mirror box.
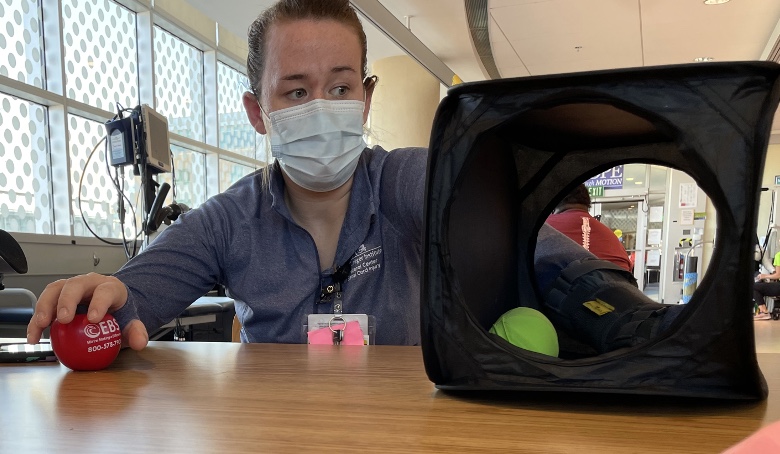
Figure 2. An example of mirror therapy.
The client is doing a simple exercise of grasp and release in this video.
Video 4
The focus of this intervention is that the patient gets feedback on what the affected hand should be doing. We do not worry about what the unaffected hand is doing in the mirror box.
We most likely are going to fatigue the affected arm quickly, so keeping things simple is ideal. They can grasp and release objects, reach for things, or perform simple tendon glides.
This intervention can be used as a preparatory exercise for other interventions as well.
Task-Specific Training
- Components
- Ensuring the task has intrinsic value to the patient
- Presents a just-right challenge to the upper limb
- Movement repetition is key to promoting functional improvements
- May be more beneficial when paired with an adjunct therapy such as electrical stimulation
Task-specific training focuses on tasks that have an intrinsic value to the patient to increase motivation and active participation in therapy. It presents a "just-right" challenge to the affected upper limb. The task is constantly monitored to increase or decrease the challenge to prevent client frustration.
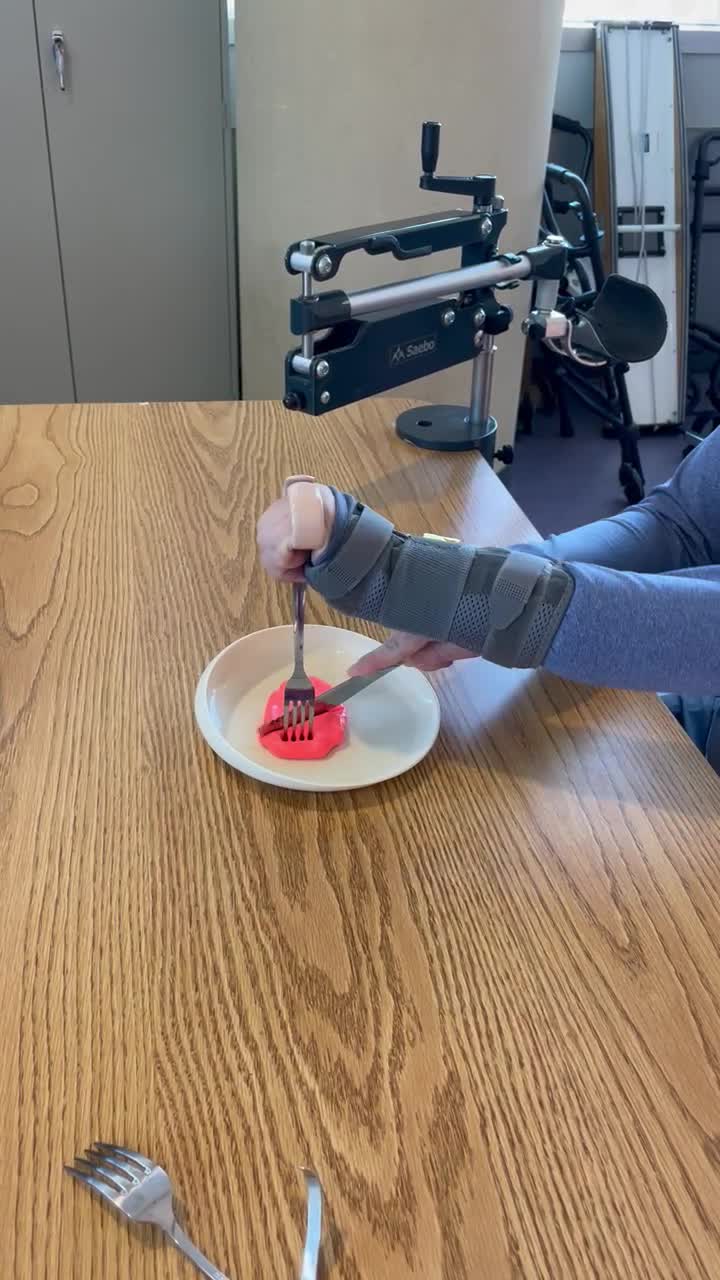
The mass practice of movement patterns is key to promoting functional improvements. E-stim can also be added. Self-feeding is an example of a task-specific activity. In this specific example, the client works towards increasing independence prior to the actual task of eating. When using this intervention, we may have the client start using a buildup handle, as seen in Figure 3.

Figure 3. Example of a built-up handle.
In video 5, we are working on cutting various foods to increase independence at restaurants and decrease her reliance on caregivers.
When using this intervention, we might have the client start by using some type of buildup handle. You will see her using a U-cuff that is added to her fork. The idea is that we are going to be monitoring her for use of adaptive equipment or trialing new things. She also has a curved plate with Dycem underneath the plate.
We can practice cutting using real food, theraputty, and Play-Doh. We can also perform this intervention in sitting and standing and move into the kitchen if available.
Video 5
We have another video (Figure 6) showing a preparatory activity working on calming down tone before doing an actual task. Weight-bearing is a great option, and we will talk a little more about this later.
The client is using a rolling pin and weight bearing while moving the shoulder moving up and down, up and down. This activity was chosen by the patient because she was able to tell me that to calm down her spasms, weight-bearing is beneficial. She is also wearing her own orthotic to keep her wrist even more stable.
Video 6
Neuromuscular Re-education
- Series of Therapeutic Techniques to Restore Normal Motor Function
- Weight-bearing
- Manual techniques
- PNF
- Therapeutic handling
- Postural training
Neuro re-education is a series of therapeutic techniques to restore normal motor function. It can be used to achieve goals of coordination, balance, postural control, and proprioception. This can be done by weight-bearing using all four limbs in combination, prone and quadruped, as you see in Figure 4.

Figure 4. The client is prone on elbows and in a quadruped position.
Weight-bearing is loading across a joint to promote the proper joint alignment and muscle co-contraction. Manual techniques are part of neuro re-ed, and this can assist the patient in getting the input of the joint moving for proper kinematics. For example, this could be facilitating scapula humeral rhythm to increase shoulder movement or PNF techniques (diagonal D1 and D2 patterns) to increase the range of motion and simulate the movements performed in daily life.
Therapeutic handling can assist in joint approximations of key points within the body to inhibit or facilitate postures and/or movement.
Postural training is challenging the patient in various balancing activities and environments to correct posture and maintain an upright balance.
Figure 4 shows different pictures of what weight-bearing can look like in prone and quadruped. You can also do weight-bearing in toe kneeling, standing, and sitting. If the patient has an unstable joint, a shoulder subluxation, or general weakness, the therapist can assist in joint approximations, use splints, or e-stim, if that is helpful.
Video 7
This video is trying to show you an example of what therapeutic handling could be like through joint approximation.
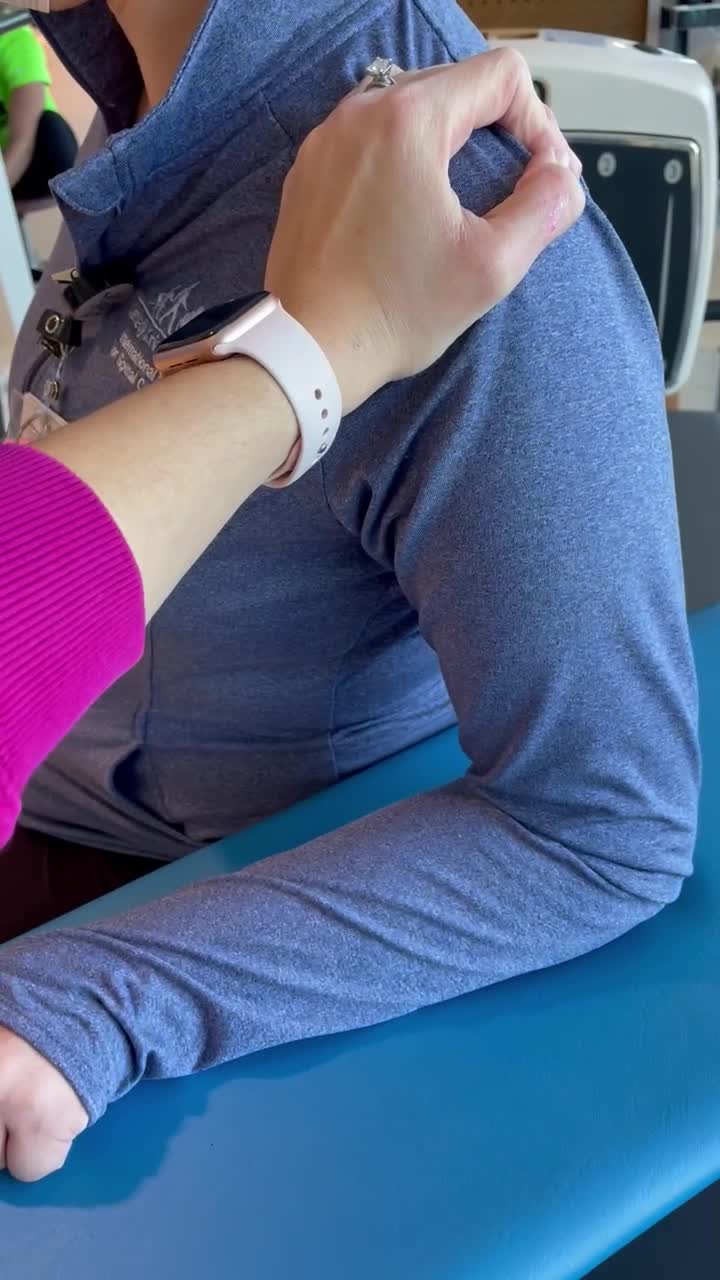
This is not the best video, but I am trying to show a therapist approximating the shoulder joint while the client is laterally weight-bearing onto a bench. The therapist could move posteriorly behind the patient to have a better handle on the shoulder. Then, they could assist with the postural alignment and give cues to the patient as she shifts weight onto the arm and moves back upright. I would also have the patient slow down these movements. A mirror could also provide visual feedback to the client.
Video 8
This is just another example of dynamic weight-bearing with the patient.
She is using robotic equipment called the PABLO. This activity can be completed in sitting, standing, prone, and quadruped. I am using a grip assist on the left side to focus on her proximal shoulder strengthening and get dynamic movements.
Functional Electrical Stimulation
- Application to a Paralyzed or Weak Muscle to Achieve a Specific Muscle Function
- Benefits
- Increase in muscle strength
- Improve shoulder subluxation
- Reduce muscle tone
Next, we move into functional e-stim, which is the application of e-stim to a paralyzed muscle to achieve a specific muscle function. The benefits include increasing muscle strength, improving shoulder subluxation, and reducing muscle tone.
Per PT clinical guidelines, FES can increase gait speed, mobility, dynamic balance, walking endurance, muscle activation, and quality of life.
There is a range of devices that clinicians can use for FES, and each device has its own set of parameters, including pulse width and frequency. This can assist with producing a muscle contraction, sensory stimulation, or decreasing pain or tone reduction. It is important to note that OTs can only use this device if they have a certification, and there is a course for that.
Figure 5 is an example of a setup of e-stim that is used with a client.
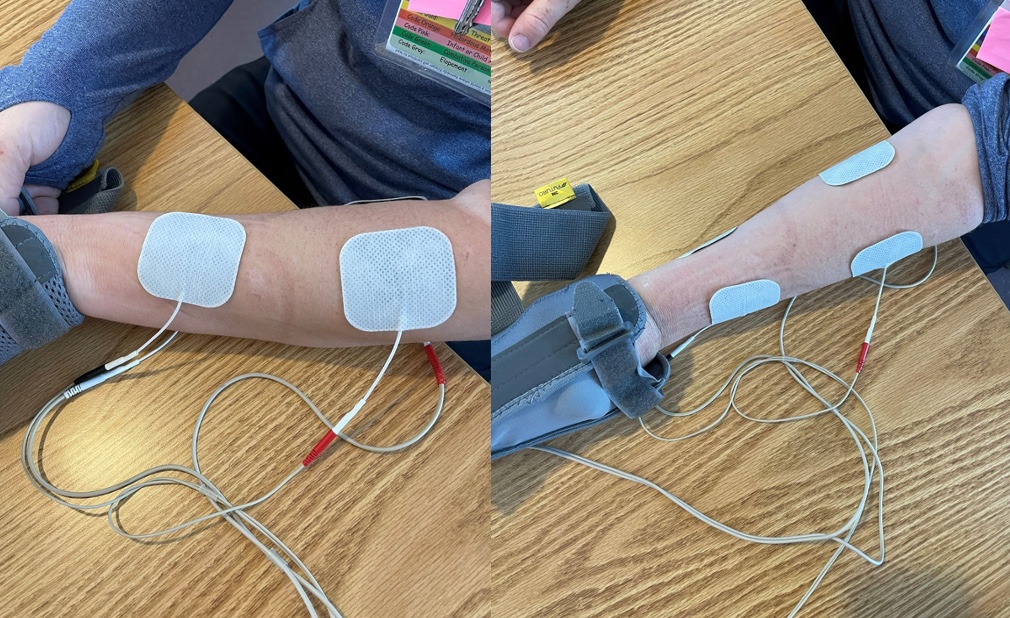
Figure 5. Client with FES application.
With this type of device, we can use a pre-programmed setting for the flexors and extensors as an example. When I press the trigger, it will then open her fingers. We have a video of her using this (Video 9). I am pairing FES with a functional grasp in a release task and prepping her ability to pick up items used for grooming.
I also have her in a mobile arm support to help unweight her shoulder and give her a little bit of support. I initially set up her forearm flexors and extensors with the trigger. However, once her forearm flexors were turned on, she could not extend her fingers out of the fist. We discussed this with her, and she was able to direct us to do something different. Often, patients know what works for their bodies. In fact, she said when she had a bad day, flexion of her fingers would overpower other movements, and she couldn't come out of it for a little bit.
Instead, we shut off the stim, and she took a break. We worked on weight bearing through her fingers.
Video 9
You see me trying to give her the ball, it is not perfect. The more practice, the more effective strategy can be determined.
Aquatic Therapy
- Provides an Environment for Challenging Activities
- Benefits
- Buoyancy
- Thermal
- Resistance
Aquatic therapy is a great intervention that allows the patient to explore his or her own body in a safe environment. It allows for more challenging activities due to the benefits that the water gives. One benefit is buoyancy, which decreases the amount of weight-bearing. It also helps to grade an activity.
Thermal benefits can also increase the person's heart rate, stroke volume, and cardiac output, which can also reduce tone, promote relaxation, and increase endurance.
Water resistance provides strengthening opportunities that might be more challenging on land. For instance, PTs can use more challenging and longer bouts of local motor training while in an aquatic setting. OTs can focus on the upper extremity, core, and trunk strengthening. We can do these activities in different positions, such as supine, sitting, standing, and modified prone.
It is important to note that not all clinics have aquatic therapy. My clinic does, which is why I am including this here. There are also aquatic therapy places in the community.
When you first get a patient into a pool, it might take a session or two for you and the patient to understand how their body moves. They might not have been able to move their body this way in quite some time, especially if they have been in rehab for a long time.
Gait Training
- Clinical Practice Guideline
- High Intensity
Katie: The level of ambulation following stroke is a long-term predictor of participation, which is why we wanted to talk about it here.
There is a clinical practice guideline for PTs for improving locomotor function in patients with chronic stroke that I wanted to highlight here. For chronic stroke, we are talking about patients greater than six months post-stroke. To improve gait parameters, such as walking speed and distance, utilizing high-intensity gait training and virtual reality coupled treadmill training is strongly recommended. By high-intensity gait training, we mean mass locomotor practice at high cardiovascular intensities or 70 to 80% of their age-predicted heart rate max. Virtual reality coupled treadmill training is walking on a treadmill with a VR headset to increase engagement and goal-directed tasks.
Outpatient Therapy: Barriers
- Spasticity
- Contractures
- Movement Disorders
- Cognition
- Caregiver Support
- Home Set-up
- Coping/Mental Health
Alaena: There are many barriers in the outpatient setting, including spasticity, contractures, movement disorders, cognition, caregiver support, home setup, coping, and mental health.
Spasticity
- Problem Solving
- Inhibiting vs. facilitating
- Medical vs. therapy interventions
- Interventions
- Prolonged stretching
- Vibration
- Weight bearing
- TENS
- Manual techniques
- PNF
Spasticity can create problems for motor functioning, and limit range, coordination, and positional movements. When talking about spasticity, it is good to figure out if that spasticity is inhibiting or facilitating the goals of the patients. For example, if a patient has lots of extensor tone, this may help the client to be more independent with stand pivot transfers.
Before you start your interventions, you want to investigate any medical interventions, like Botox. However, a patient will be dependent on receiving Botox every couple of months to maintain benefits. The downside of this intervention is that a patient can lose functional movements, such as a grasp and release. If you put Botox in their flexors, as an example, they might become less functional in ADLs.
Therapeutic interventions include prolonged stretching, vibration, weight-bearing, TENS, manual techniques, and PNF. It is always good to be in communication with your counterpart and medical provider to determine how spasticity is affecting their sessions, and if there are options to manage the spasticity more effectively through a medical perspective.
A vibration plate can be used in standing, in prone or quadruped, or in an anterior or lateral prop. This is an example of an upper limb one in Figure 7.

Figure 7. Example of a vibration device.
This is called a smart dumbbell that has a range of frequencies from 5 to 40 hertz. Higher frequencies facilitate muscle strength, and the lower ones reduce tone. You can use this in a static or dynamic way. If you are working on grasping, you could have them just hold the device. If we are trying to decrease spasticity or tone at the biceps, active movement may be beneficial. Again, every patient is different so you will want to try different movements and positions. J
Skin breakdown can be a concern, especially with a patient that has never used vibration. You should use it for a short duration first and then check the skin.
Contractures
- Problem-solving
- Medical vs. therapy interventions
- Functionality
- Therapy Interventions
- Splinting
- Serial casts
- Weight-bearing
- Stretching
Contracture is another barrier that we see in the outpatient setting. Again, I am going to ask if there are any available medical or therapeutic interventions that the patient has trialed and if they were beneficial. I also want to know what the functionality of the contracture is. Even though a contracture can sound scary, our patients get creative as they may have had this diagnosis for a long time. We may even see less functionality if we take away the contracture. Problem-solving with them is important.
Interventions can include splinting, serial casting, weight-bearing, and prolonged stretching. There was a study in 2020 by Lecharte where he followed patients with chronic strokes for six weeks on a stretching protocol, and they saw no effectiveness. Do we need to see longer protocols for stretching, or is stretching not effective? The verdict is out on that.
Movement Disorders
- Problem-solving
- Inhibiting vs. Facilitating
- Medical vs therapy interventions
- Prior interventions
- Therapy Interventions
- Weight-bearing
- Biofeedback
- Mirror therapy
- Virtual Reality
Movement disorders are another barrier that may inhibit rehab for stroke patients. Post-stroke movement disorders have been observed in 2 to 4% of stroke patients, but research is limited. Typically, these disorders inhibit rather than facilitate; however, everyone is different. Discuss with the client about medical interventions they have tried, like weight-bearing, biofeedback, mirror therapy, or virtual reality.
Cognition
- Problem-solving
- SLP involvement
- Level of impairment
- Caregiver and patient understanding
- Restorative vs compensatory
Cognition is another barrier. If speech therapy is not involved, OT can help out with performing some extra cognitive assessments to tease out the specific cognitive impairments. Once we can understand what that impairment is, we can decide on a restorative, compensatory, or combined approach. A restorative approach will focus on repetitive tasks that are simple and graded, including performing in various environments and adding extra layers to that task. A compensatory approach includes verbal cues, phone reminders, and visual cues, such as red tape, to facilitate scanning in environments. They can also use visual schedules and the environment can be modified, like the removal of tripping hazards, such as a throw rug.
Caregiver Support/Home Setup
- Problem-solving
- Support available
- Home accessibility
- Previous home therapies
- Therapy Interventions
- Advocacy
- Education
- Strategies
- Collaboration
We can also discuss with the patient and caregiver to see what their level of understanding is. Is the patient aware of the deficit that he or she has? Does the family member understand it? Is safety a concern? Since outpatient is geared toward more specific goals, it is important to understand caregiver support and home accessibility. Once clients start their outpatient journey, their caregiver support may have changed due to the prolonged duration of their diagnosis and/or issues with insurance and funding.
As I said before, COVID has severely impacted patients' consistent caregiver support. Their homes may also not be fully accessible. Maybe during their acute and inpatient stay, the patients were able to report the ability to stay on a first-floor setup, but once home, they realized that it was not feasible.
We also want to know if the patients have had any home therapy. If so, what were their recommendations, and what did they work on?
Interventions include educating patients and families, advocating for the patient if able, and strategies to increase independence within their home environment. We can encourage the patient and caregiver to take pictures of the home setup. Doing a telehealth visit to get the full picture of the home can be helpful, if appropriate.
Lastly, we want to collaborate with our PT or OT counterpart to make sure we are both on the same page, especially for recommending equipment and creating a home exercise program.
Coping and Mental Health
- Coping (Rapoliene et al., 2018)
- More than 50% of survivors remain temporarily or permanently disabled
- Only 20% of survivors return to work
- Motivation affects outcome
- Depression (Tsao et al., 2022)
- Approximately 1/3 of stroke survivors
- The highest frequency in 1st-year post-stroke
- Associated with higher mortality and worsening function
Coping and mental health are still critical components of outpatient. The statistics are the same as presented in Part 1, with greater than 50% of stroke survivors remaining disabled and 80% not returning to work. There is a dramatic change in the patient's lifestyle post-stroke, and it takes time to cope. There is no set timeline for patients, so we need to be mindful that we are meeting them where they are.
We can also foster autonomy in patients by letting them take the lead in their care, and this might help with their active coping process. We also know depression is at its highest in that first year, and that is when we might see these patients. If there are any signs of mental health issues while you are treating a patient, you can advocate for them to the medical team or refer them to social work if available. You want to get permission from the patient before that happens.
You can also give resources and education to the parent, caregivers, and patients about social work and support groups (peer-to-peer if that is available), and continuing to build rapport with the patient is going to help in the long run.
Outpatient Therapy: Other Considerations
- Long-Term Plan
- OT and PT services are not enough to help people recover from stroke
- Creative complementary approaches to facilitate motor recovery, including engagement in interventions when not present in the clinic, are important
Other considerations are to encourage them to get involved in outside recreational and support groups. This is important because when therapy ends, we may see a further decline in social and physical involvement. We can give simple resources like local gyms that have adaptive programs in aquatic therapy and recreational programs.
I am in Maryland, and we have local groups that do community outings depending on the season. The volunteers usually have some rehabilitative or medical background. Activities include skiing, biking, kayaking, and water skiing.
The more you encourage them, they might surprise you. We want to set them up for success by encouraging them and giving them the resources, and then the rest is up to them and their caregiver.
Outpatient Rehabilitation: Literature Update
- Nerve transfers post-stroke for spastic UE
- UE nerve releases for spasticity management to improve gait function (AlHakeem et al., 2020)
- Electrical stimulation at wrist flexors/extensors early on (~72 hours post onset) to prevent hand/wrist contractures (Fletcher et al., 2019)
Research shows that upper extremity nerve releases for spasticity management can improve gait. They are also researching the earlier use of e-stim, typically 72 hours post onset of stroke, to prevent contractures. However, the research that is out on the e-stim right now is a very small sample size. It is also harder to implement that protocol in acute care because of the complexities and the medical needs of the patient.
Outpatient Rehabilitation: Interdisciplinary Approach
- Screening for Other Disciplines
- Communication
- Education
- Supporting Other Disciplines
- Return to Work/Community Reintegration
Overall, OTs and PTs can work together in many ways in the outpatient setting. Examples can be for screening the other disciplines, especially if the patient is only receiving one therapy while at a PT or OT-only clinic. We can collaborate with our counterparts by observing actions such as bed mobility or sitting balance for PT and conversing about what we are seeing, and vice versa.
It is important to note that because of fatigue, tone, and other issues, patients might present differently in PT versus OT sessions. Communication becomes crucial, and this can be done via a simple email or a Post-it note.
We want to provide education to the family and ensure that the DME we are recommending fits inside the house from PT and OT standpoints.
Again, we want to support other disciplines. For example, we can use upper extremity management or weight-bearing techniques during PT or add standing balance tasks during OT. As stated earlier, these can be simple additions to the therapy program. For example, if PT is working more on standing or ambulation, maybe OT can take over the sitting balance and work on that for core trunk strengthening needed for seated ADLs.
We want to assess work and community reintegration. Education and encouragement may help motivate the patient to try out a new activity. We all have different experiences, so having those one-on-one conversations with our patients might motivate them to try something out.
Outpatient Rehabilitation: Case Study J.K.
- J.K. received home health therapy x 6 weeks. Upon transition to outpatient therapy, J.K. is 12 weeks post-stroke. She takes mobility services to outpatient appointments with caregivers.
J.K. takes mobility services to outpatient appointments with a caregiver. She can now ambulate short distances with supervision with a standard point quad cane and uses a wheelchair for longer distances. Her left arm is three minus and grasp and release of two; the left lower extremity strength is four out of five. She has coordination issues. She also only attends to her left side 50% of the time without cues and uses a written schedule during the day due to short-term memory deficits.
- Current Status
- ADLs: supervision for basic ADLs with significantly increased time and setup
- IADLs: min A for locating items, safety, and mod A for newer tasks
- Mobility: supervision for safety with gait and stairs due to L inattention
- Falls: 2 falls over the past 4 weeks
- Patient Goals
- To be able to go grocery shopping independently
- To be able to take care of herself so her caregiver can return to her own home
- To be able to return to her weekly walking club so she can socialize with friends
She requires supervision with basic ADLs, min assistance for locating items, and supervision for mobility. She has had two falls over the past four weeks. The patient wants to be able to go grocery shopping, take care of herself so her caregiver can return to her own home, and return to a weekly walking club so she can socialize with friends. These are all great goals. Although they might not align with what OT or PT wants to work on at the moment, these are important as they are the eventual end goals of this patient.
OT/PT Goals
- Examples of Possible OT Goals:
- Patient will be able to grasp and release 3-inch balls to a target in 3 out of 5 trials independently in prep for independence for opening/closing doors to access the community
- Patient will independently be able to locate all items needed for simple meal prep independently
- Patient will be able to reach 3 out of 5 items placed on table using left UE in prep for independence needed for dressing
- How Can PT Help Facilitate These OT Goals?
- Add grasp/release with exercises using weights, opening/closing doors
- Environment scanning during obstacle courses
- Reach with left UE during dynamic balance training
Here are some sample OT goals, including grasp and release for opening and closing doors to access the community. It could also be independent grasp and release to be able to hold onto a toothbrush or different size jars when opening them. Other goals were to locate items for simple meal prep and to reach three out of five items on a table.
How can PT help facilitate these OT goals? PT can maybe add some grasp and release by adding dumbbells or practice opening doors prior to their session. They can also add environmental scanning during obstacle courses and incorporate more reaching during dynamic standing or sitting balance.
- Examples of Possible PT Goals:
- Patient will negotiate obstacle course consisting of static and dynamic obstacles of various heights and uneven surfaces independently x 3 consecutive repetitions in order to improve dynamic balance and attention to L environment during functional tasks
- Patient will ambulate on treadmill x10 minutes without rest breaks at speed >2mph for improved endurance to be able to access community
- Patient will negotiate 1 FOS with single HR independently, requiring no cues for safety in order to access her home
- How Can OT Help Facilitate These PT Goals?
- Navigating obstacles during OT task setup
- Locating items throughout session strategically placed on left side
- Standing balance tasks and ambulating throughout sessions
Examples of PT goals include negotiating obstacle courses with various heights, ambulating on a treadmill to build endurance, and then negotiating one flight of stairs independently. OT can help by having them navigate obstacles during OT setup and having the patient go and grab the materials needed that are strategically placed on the left side. They can also work on standing balance and ambulating throughout the session.
Interventions
- Interventions
- Aquatic therapy
- Stretching
- Strengthening
- Balance training
- Robot-assisted therapy
- Neuromuscular re-education
- CIMT
- Orthotic management
- High-intensity gait training
This is not a conclusive list but a list of examples for therapy. Aquatic therapy can bring awareness to their left side in a safe environment and focus on upper and lower extremity coordination, stretching and strengthening to maintain good length of joints, proper kinematics, increasing strength to uppers and lowers, balance training needed for community outings, and various IADL tasks. Robot-assisted therapy can focus on specific upper and lower extremities muscles to increase coordination, strength, and awareness of the left side. Neuromuscular re-education can increase sensory awareness and strength to the left side. OT might be working on incorporating a modified CIMT approach or using orthotics, and PT could focus on high-intensity gait training to increase coordination and strength.
Outpatient Rehabilitation: Community Reintegration
- “An estimate of more than 30% of stroke survivors have persistent deficits in autonomy, engagement, and fulfilling societal roles” (Gittler & Davis, 2018)
Our goals for our patients are that we want to get them back to living their best lives. Upon discharge, we want them to flourish, even though it can seem scary at times. Sometimes the best we can do as therapists are to educate, motivate, encourage, and give them all available resources. We also want to let them know that we are here to help them via email or during their next care visit.
A statistic that we found showed that more than 30% of stroke survivors have persistent deficits in autonomy engagement and fulfilling societal rules. It is important to note that every state has resources available for patients and to be more aware of what your state has to offer.
Outpatient Rehabilitation: Community Resources
- Day Programs
- Support Groups
- American Stroke Association
- Adaptive Sports
- Accessibility Lines
- Local State Assistance
- Return to Driving and Work
Some states have day programs that assist with caregiver burnout and may offer some therapy in group settings. This can be a safe place for the patient while the caregiver is at work. The American Stroke Association is a great resource to help find local support groups in your home state for the patient and/or the caregiver.
Adaptive sports might be found through local therapy clinics or through the city or state. For example, in Maryland, we have a local group called BARS, which is the Baltimore Adaptive Recreational Sports. They provide those weekend options for kayaking, water skiing, and skiing.
Different organizations may offer information on accessibility, adaptive equipment, meal programs, and home health services.
Outpatient Rehabilitation: Return to Work
- Loss of Identity, Social Isolation, Financial Hardship, and Family Stress
- Barriers
- Occupation-based approaches focus more on ADL independence and less on community reintegration, largely driven by payer policies
- Problem-solving with Therapists
Patients often talk about wanting to return to work. When they lose the ability to work or do not return to work, they lose a sense of themselves, and it can create social isolation, financial hardship, and family stress.
Therapists do not do a great job of addressing what they need to do to get back to work, as we are so focused on ADLs and mobility. Having this conversation at the beginning of our sessions can help set the stage to work toward this end goal. Can they go back to the same job, or does it need to be something different?
In Maryland, we have local organizations that help patients with returning to work and advocate for the patient to perform their jobs effectively.
Outpatient Rehabilitation: Driving Rehabilitation
- Assessments to Predict Driving Capability
- Stroke Drivers’ Screening Assessment (SDSA)
- Tabletop tests with Useful Field of View (UFOV)
- Dot Cancellation Test, Compass Test, and Road Sign Recognition Test
- Stroke Drivers’ Screening Assessment (SDSA)
Driving rehabilitation is a specialized field. It might take some research to identify local support groups and programs. There may also be wait times to get into these programs because they are so scarce. I did find some assessments that OTs can use to address problem areas, such as processing speed, divided attention, and selective attention. If the patient has processing speed issues, we can figure out how we can incorporate something into our session to help increase their independence in the deficit area.
Outpatient Rehabilitation: Case Study J.K.
- J.K. has been attending outpatient therapy for one month and has reported a desire to drive, go back to work, and explore other adapted recreational programs.
Lastly, we are back to J.K., who is still attending outpatient therapies. She has reported a desire to drive, go back to work, and explore other adaptive recreational programs. We can offer education on available recreational programs. We can also educate them on what the state guidelines are for reporting stroke to the BMV and ensure they are cleared by their doctor for driving. We can reach out to their doctor if appropriate and help them have that conversation. We can also look into programs available for driving rehab and return to work and maybe get a social worker involved.
If there are any mental health issues, this might inhibit the patient to participate in treatment. Again, we can look at peer-to-peer groups or other resources in the community.
Additional Case Studies
Case Study 1
- 62-year-old male s/p large R basal ganglia ICH. Patient with recent acute care stay x4 weeks with course complicated by high ICP’s, seizure, and decreased level of consciousness; patient s/p decompressive craniectomy, trach, and PEG. Patient discharges home after a four week stay at SAR following 1-step commands ~50% of the time and requires max A for all mobility and ADLs.
Kate: Case study 1 involves a 62-year-old male after a large right basal ganglia intracranial hemorrhage. The patient had an acute care stay of four weeks and a complicated course. He had high ICPs, seizures, decreased level of consciousness; he had a decompressive craniectomy, a trach, and a PEG. He was discharged home after a four-week stay at a subacute rehab. He is following one-step commands but only 50% of the time, and he requires max assistance for all mobility and ADLs. We are looking at a low-level patient here.
- Home Health PT/OT Consults
- Supportive family, 1st-floor setup
- Hoyer lift, wheelchair, hospital bed
- Discussion Points
- Evaluation
- Plan of care
- Interdisciplinary approach
We find that he has a supportive family and a first-floor setup. He was sent home from the subacute rehab with a Hoyer lift, a wheelchair, and a hospital bed.
Evaluation for this patient is going to include assessing for contractures, looking at skin integrity, communication, upright tolerance, and seating and positioning. We want to get him into a wheelchair and look at his seated posture. We also want to discuss patient and family goals, screen for depression, and assess his current home setup. We want to see if there is anything that could be changed to help him be more independent.
He is pretty low-level, so we need to focus on contracture prevention and positioning, a turning program, and a seating schedule to prevent skin breakdown. We also want to ensure that the caregivers are properly using the equipment properly. Can they use the Hoyer lift? Are they locking the wheelchair brakes before transferring?
We want to progress any mobility or ADL tasks for this patient to improve his overall independence.
From an interdisciplinary approach, we want to communicate with the nurse who is overseeing this patient to discuss skin integrity concerns, the equipment that he has, and the potential need for a home health aide. PT and OT should provide a united front when it comes to skin integrity, including turning and seating schedules.
PT and OT should also coordinate home exercise programs. With a patient like this, there is no way that the family is going to be able to perform a full-body range of motion or strength program. We want to provide them with a home exercise program that is doable for them so that they are not overwhelmed and can manage to do it daily.
- 62-year-old male s/p large R basal ganglia ICH, presents to outpatient PT via referral from MD for back and bilateral shoulder pain eight months post-stroke. The patient uses a community mobility program for transportation.
Fast forward a couple of months, this same patient is now in outpatient PT, and he was referred by his doctor for back and bilateral shoulder pain. He is eight months out from his stroke and is using a community mobility program with his caregiver for transportation to the clinic.
In this chronic phase, he has had therapies, subacute rehab, and home health therapy, and then he was discharged. If he was recommended for follow-up, he did not go. Now, we are seeing him eight months later in a PT clinic with these findings.
- Eval Findings
- Worsening back pain in the lumbar and thoracic spine
- L shoulder pain in supine and seated
- Worsening spasticity throughout
- R shoulder pain with movement
- Discussion Points
- Need for outpatient OT?
- Accessibility
- Addressing pain
He had worsening back pain in the lumbar and thoracic spine and shoulder pain on the left side in supine and seated. He has shoulder pain on the right with movement and worsening spasticity throughout.
Does he need outpatient OT? From a PT standpoint, we are going to assess his shoulders and talk about his daily activities. What is he doing? Is he getting out of bed or not? Has he been doing his home exercise program? What has changed, or what is a potential cause of these worsening issues? Likely doing less without regular therapy follow-up is an issue, and he is going to need strengthening and ADL practice. OT can also focus on spasticity and upper extremity pain in this patient.
I would like to make a quick note about accessibility for this patient. He is low-level, uses a wheelchair, and gets from the bed to the wheelchair via a Hoyer lift. He has to rely on transportation programs because he needs a wheelchair van to get to appointments. It is difficult for him to get to appointments. If we are now involving occupational therapy, is this patient appropriate for outpatient therapy at home, or should he go to a clinic that offers both services so that transportation is not as big of a barrier?
Our last point is addressing pain. Why might a patient like this have pain? The most likely cause is related to positioning and non-use. We need to look at how he is sitting in his wheelchair. He is likely flexed forward and maybe leaning.
It turns out that this patient had lost weight in those eight months since he got his wheelchair, and it was not fitting well. We want to ensure that we refer him to a wheelchair clinic or back to his vendor for an updated seating system. The other position that he is in most of the day is his bed. Can we simulate it in the clinic? Can the caregiver take a picture of him in his bed several times during the day so that we can see what is going on? Positioning is hard in a hospital bed, and he likely slides down in a flexed posture all day. We can problem-solve with the caregiver on how to get him in a proper position. For example, can they set an alarm to address his position every hour or two, or can they start a seated or turning program?
Case Study 2
- 87-year-old female s/p R PCA stroke with left-sided weakness, left inattention, vision deficits, and decreased safety awareness. The patient has good family support and will have 24/7 care from family members. The patient ambulates with CG/min A due to safety. A home safety evaluation with home health services after discharge from acute rehab was recommended.
- Discussion Points
- Interventions
- Home modifications
- Education
The case study is an 87-year-old female, status post right PCA stroke with left-sided weakness, left inattention, visual deficits, and decreased safety awareness. She has good family support with 24/7 care from family members. She ambulates with a contact guard to min assistance due to safety. It was recommended that she have a home safety evaluation with home health services after discharge from acute rehab.
Would you recommend home PT and OT? Before selecting any of these interventions, it is important to know the patient's and family's goals as well as the home setup. Interventions in acute care rehab most likely focused on strengthening the upper extremity and gait training and stair training from a PT point of view.
We should focus on educating the family on what makes the home safe. Although the patient went to acute rehab, we are still recommending a home safety eval as well as 24/7 care due to her age and safety issues. We may need to make some home modifications, recommend specific DME, or set up visual compensatory strategies, such as adding motion sensor lights, door alarms, visual schedules, and tape for scanning. The home evaluation will be helpful to help with that modification.
The other modifications that we could think about are a stair lift so the patient does not have to use stairs as much and any other low-level things like grab bars and shower chairs, which are reasonably priced at stores or on Amazon. Other chairs can be set up around the house for endurance.
We need to educate the family about why we are recommending this 24-hour care due to decreased safety awareness, visual deficits, and left inattention.
Summary
- Interdisciplinary Approach to Stroke Rehabilitation
- Benefits
- Ways to implement
- Possible in all settings
We have a few more case studies that we left in this presentation for you in the handout. The idea with these case studies is that we are not giving you specific information. We want you to go through them and think about the discussion points we have discussed. Think about the questions that you have about these patients. If you have additional questions after you go through the case study and would like to talk about it, we are here.
Overall, an interdisciplinary approach to stroke rehab is beneficial, as it optimizes recovery, provides client-centered care, educates on energy conservation strategies, and provides good time management for the therapist.
There are many ways to implement this approach. You can verbally talk to your counterpart, send a quick email, attend medical rounds, and implement different techniques into your own sessions to support the other discipline. Again, these do not have to be massive changes; something small can have a valuable outcome.
Lastly, this approach is possible in all settings. We discussed how we could effectively work together to get that patient home as safely and quickly as possible. Although it might look different in each setting, it is about getting creative to optimize patient outcomes.
Questions and Answers
Are Baclofen injections suitable for spasticity in home health populations, or does it make an elderly person too drowsy?
Baclofen injections do have side effects of drowsiness, and each patient is going to respond differently to these localized injections. The patient needs to talk to their doctor about the different options. Oftentimes in older adults, Botox can be used in place of baclofen to prevent the drowsiness side effect. We also have to ensure that whatever the doctor recommends does not negatively affect other meds.
How quickly do you see improvement with stimulation for a subluxation?
This presentation specifically looked at the subacute and chronic populations. Because of that, we see slower gains in this population. You also do not use stimulation as a stand-alone treatment. Every patient is different, and there is no black-and-white answer to that question. Stroke is such a gray area, and you can have two people with the same diagnosis and presentation, but one shows improvement and one does not.
If you have a patient that is asking about improvement, you can try to use a quantitative assessment that shows small improvements.
What about Kinesio taping?
The research is limited on Kinesio taping. It is an intervention that needs to be done frequently, and the patient or caregiver needs to be able to reapply if it comes off.
Again, it is not a one-and-done for everyone, so I would recommend trialing different things. What I typically like to do when I work with my outpatient patients is trial one or two new interventions to see if there is any improvement.
Are there any activities or exercises that we can incorporate to encourage recovery and prevent mini-strokes?
There is a high prevalence of TIAs. The activities and exercises that we use to treat patients with TIAs are going to look exactly like the exercises and activities we use to treat patients who have had an ischemic or a full hemorrhagic stroke.
As far as preventing recurrence in these patients, we need to make sure that they are following up with their doctors. When you have a TIA, your risk of having a stroke is elevated. To prevent a reoccurrence, we need to ensure that they are following up with their doctors, monitoring their blood pressure, and taking their medications. No therapy intervention will prevent a stroke.
Are there cognitive assessments for return to driving?
There were some Australian studies that highlighted Stroke Drivers’ Screening Assessment (Australian Version). This tabletop test is for a useful field of view, processing speed, divided attention, selective attention, and to tease out any other cognitive deficits.
There is also an array of cognitive assessments that focus on quantitative gains and a task analysis of what that patient needs to be able to drive.
References
See additional handout.
Citation:
McCool, A., & George, K. (2022). Interdisciplinary approach to stroke rehabilitation: Outpatient, home health, and community rehabilitation phase. PhysicalTherapy.com, Article 4859. Available at www.PhysicalTherapy.com

